ARTICLE
Vol. 133 No. 1510 |
Use of rehabilitation after hip and knee replacement in New Zealand: a national survey
Long-term outcomes following primary hip and knee joint replacement are favourable with most patients experiencing positive functional outcomes over time.
Full article available to subscribers
Long-term outcomes following primary hip and knee joint replacement are favourable with most patients experiencing positive functional outcomes over time.1,2 However, up to 30% of patients following knee replacement and a smaller number of those following hip replacement report little or no improvement with respect to ongoing pain, restricted range of motion and unsatisfactory function.2–4 There may be differences in recovery depending on type of joint replaced. For example, it is generally agreed that individuals take longer to recover and require more rehabilitation following total knee compared with total hip and uni-compartmental knee replacement.4–6 Various demographic and clinical factors may influence these outcomes. These include age, gender, general health and comorbidities, post-operative complications, surgical wait time and use of rehabilitation.1,4 The latter is the focus of this study.
Rehabilitation, particularly exercise-based physiotherapy is generally accepted as standard before and after hip and knee replacement7,8 and is a set of interventions designed to optimise functioning and reduce disability.9 However, protocols for rehabilitation before and after joint replacement vary widely across studies and countries and the optimal mix of setting, mode and intensity of rehabilitation remains unclear.10,11 Pre-operative interventions include a focus on education and an opportunity to address physical and psychosocial issues that may impact on surgery outcomes, such as anxiety and depression, pain management, nutrition, smoking and exercise expectations.4,12 Rehabilitation in the post-operative phase can include occupational therapy and physiotherapy to target pain management, levels of activity, participation and quality of life.4,13
There are a small number of published studies characterising rehabilitation services used by patients before and after joint replacements in some countries such as the US.14,15 However, in New Zealand little is known about the extent to which hip and knee replacement patients receive rehabilitation care and how use of rehabilitation varies on the basis of ethnicity. For example, while the issues are complex, differing rates of joint replacement uptake may be possible between Māori and non-Māori, consistent with two published studies we could find;16,17 however, no studies have considered whether there is variability in terms of use of rehabilitation before and after joint replacement on the basis of ethnicity. Use of rehabilitation services may also be impacted by economic barriers,18,19 where access to health services might depend on where a person lives and access to funding for services.20
Study objectives
The objectives of this study are to: i) describe the extent to which New Zealanders use rehabilitation before and after joint replacement, and ii) to consider whether there is variation based on geography and ethnicity.
Methods
Study design and recruitment strategy
The role of rehabilitation (ROR) study is a cross-sectional questionnaire-based study investigating the use of rehabilitation before and during the first six months following primary total hip or knee, or uni-compartmental knee replacement in New Zealand.
Participants were recruited from the New Zealand Joint Registry (NZJR) in order to achieve a national sample with geographical diversity. Because of the large numbers of registered primary hip and knee replacements, NZJR obtains patient-reported outcome information from randomly selected patients across the country to achieve an annual response of 20%. This was the sampling frame for this study. Flyers for the study were included in six-month post-operative NZJR mail outs between June 2015 and July 2016, and all patients returning flyers with their contact information were approached as soon as flyers were returned and invited to participate in the study.
The study received ethical approval from the University of Otago Human Ethics Committee (ref H14/070).
Participant selection
Patients registered and followed by the NZJR after primary hip or knee joint replacement in either private or public systems in New Zealand were eligible to participate in the study. Patients who met the following criteria were included: i) age 45 years or older, ii) underwent an elective unilateral total hip or knee, or uni-compartmental knee replacement for osteoarthritis six months prior to recruitment, and iii) agreed to participate in the study. We excluded patients with any previous operation on the index joint and any non-elective joint replacements following fractures.
Data collection
Contact information was supplied monthly from the NZJR (name, preferred contact information) for potential participants meeting inclusion criteria who had agreed to being contacted by the study team. Potential participants were then contacted within one month of contact details being made available by a research assistant to discuss the study and invite participation.
Once recruited, ROR participants completed questions in booklet form regarding timing, type, intensity and duration of any rehabilitation following referral for joint replacement (pre- and post-operatively). Demographic and clinical questions were also included. Questionnaires were available for completion either online (eg, Survey MonkeyTM) or by mail depending on the preference of the participant. Additional clinical information (procedure type, date of surgery, body mass index, comorbidity classification) was collected from the NZJR. This minimised participant burden by avoiding duplication of data collection.
ROR study variables
Demographic variables included age, gender, ethnicity, education, work status, funder (public/private insurance/self). Clinical and surgical variables included other pre-existing medical conditions/comorbidities (self-report/American Society of Anaesthesiologists (ASA) classification21); body mass index, procedure type (total hip, total knee, uni-compartmental knee) and time on surgical waiting list (weeks). Rehabilitation variables included time from surgery to first rehabilitation session (weeks); pre- and post-operative rehabilitation type (physiotherapy, occupational therapy, other), setting (home, outpatient, community centre, other), frequency of sessions per week, total hours of rehabilitation); and number of post-operative follow-up reviews with the surgeon. Outcomes were evaluated using the six-month post-operative Oxford Hip and Knee scores22,23 accessed from NZJR and a brief measure of quality of life (WHOQOL-8).24,25
Data analyses
Data were analysed using SPSSv24.0.26 First, we characterised the sample in terms of demographic status, health (eg, comorbidities, body mass index), procedure type, geographic location, funding source, participation in pre- and/or post-operative rehabilitation therapies and outcomes, using descriptive statistics. Second, for those who obtained rehabilitation services, we identified the setting (eg, outpatient, at home, community centre), time from operation to first rehabilitation session, rehabilitation duration, frequency (times per week), and intensity (minutes per session x number of sessions per week/number of weeks of rehabilitation; total hours), and how rehabilitation services and practice patterns varied on the basis of geography and ethnicity.
Bivariate analyses tested relationships between demographic and clinical variables and rehabilitation pre- and post-operatively. For discrete variables, we created contingency tables (cross-tabs) and used chi-squared tests to determine the significance of two-way associations. For continuous variables with normal distributions, Pearson correlation, two-sample t-tests, or analysis of variance were used. For variables with non-normal distributions, non-parametric tests were used including Spearman correlation, Mann Whitney U or Kruskal-Wallis tests as appropriate.
The approach to missing data was to use list wise deletion, also the default SPSS approach. We believe this was appropriate because of the sample size and the limited amount of missing data (<3%) across variables. Data presented are unadjusted with no correction for confounding variables.
Results
Seven hundred and sixty-nine people meeting inclusion criteria returned flyers to the NZJR. Of these, n=608 were successfully recruited into the study and returned questionnaires (n=158 online and n=450 by post). Figure 1 shows recruitment flow into the study.
Figure 1: Recruitment flow chart.
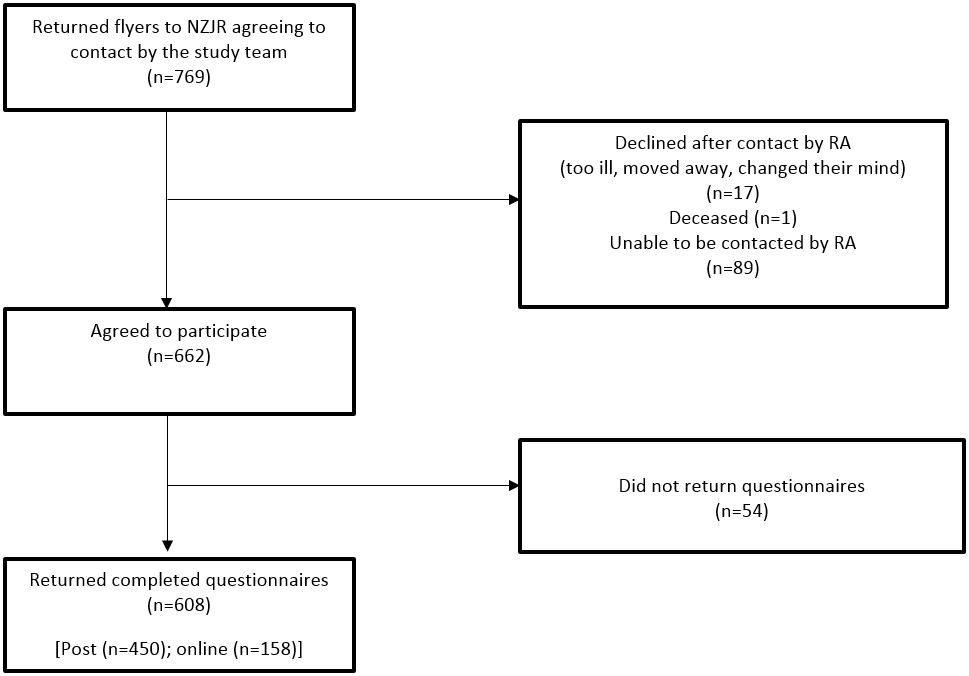
Figure 1: Recruitment flow chart.NZJR = New Zealand Joint Registry; RA = research assistant.
Description of study sample and outcomes
A summary of participant demographic, clinical and outcome characteristics is provided in Table 1. The average age of participants was 68.2 years. There were fewer men (45.2%) than women; the sample was predominantly New Zealand European (89.6%) and generally well educated, with 69.4% reporting high school- or tertiary-level qualifications. The main funding sources for surgery were private insurance or public funding, and participants waited on average six months for surgery. Evaluation of outcomes indicated a majority of participants (51%) reported an excellent outcome on the basis of Oxford scores using the 4-category set of outcomes from poor to excellent recommended by the NZJR.27 Mean level of quality of life was also high (mean WHOQOL-8 score 32.4, SD 4.9).
Table 1: Demographic and clinical characteristics of the ROR study sample (n=608).
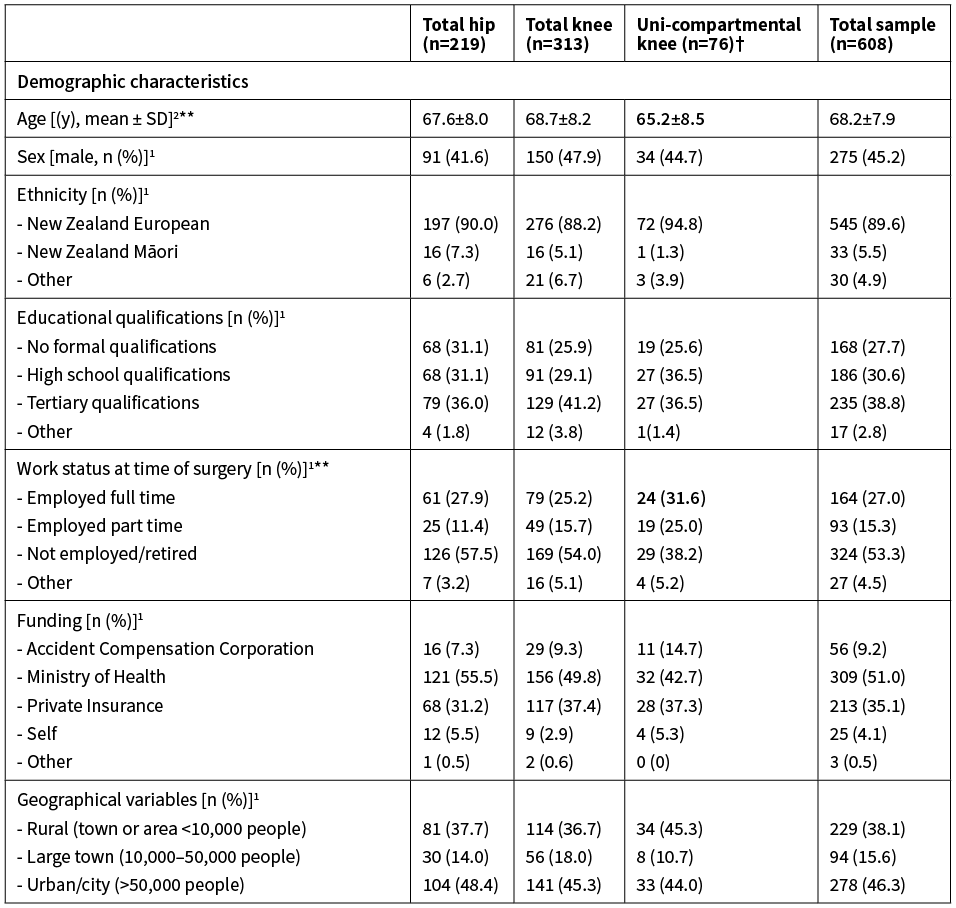
** p<0.05 (1 = Chi square; 2 = Kruskall-Wallis test). ASA = American Society for Anaesthesiologists; WHOQOL-8 = World Health Organization Quality of Life 8-item questionnaire. 95% CI = 95% confidence interval. 3. Categories from NZJR.27 Where significant, data in bold delineates where the difference lies. †Bootstrapping not completed for unicompartmental knees due to low sample size.
When demographic and clinical variables were examined by procedure type, the analyses indicated participants undergoing uni-compartmental knee replacements were younger than total knee and total hip participants (X2(2)=7.96, p=0.02) and more likely to be working at time of surgery (% in full- or part-time paid employment: uniknee 56.6; total knee 40.9; total hip 39.3; X2(8)=20.03, p=0.01). Total knee replacement participants demonstrated higher mean body mass index than total hip and unicompartmental knee participants (X2(2)=8.61, p=0.02). The only other significant difference across the three procedure groups was with respect to Oxford scores at six months after surgery with total knee participants reporting greater pain and functional difficulty than both other groups (X2(2)=7.96, p=0.01).
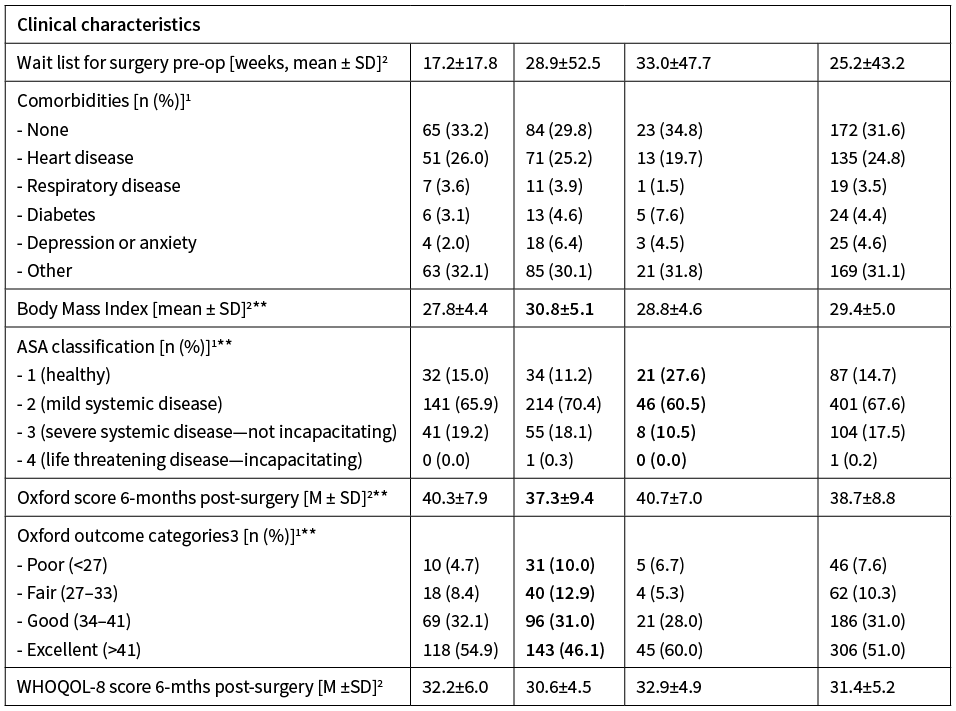
Extent of rehabilitation used (intensity, duration, type)
Table 2 shows the breakdown of pre- and post-operative rehabilitation. These analyses indicated more participants used rehabilitation, mainly physiotherapy, post-operatively (79%) than they did pre-operatively (31.0%). Rehabilitation was mostly outpatient clinic-based compared with home- or community-based (pre-op clinic-based: 56.6%; post-op clinic-based: 68.9%). Of those using pre-operative rehabilitation, although there was wide variability, participants reported an average of 8.3 weeks of intervention, 2–3 sessions a week. Of those receiving post-operative rehabilitation, participants reported waiting on average 2.5 weeks before rehabilitation commenced, with an average of 7.1 weeks of follow up, 1–2 sessions a week.
Table 2: Pre- and post-rehabilitation characteristics (n=608).
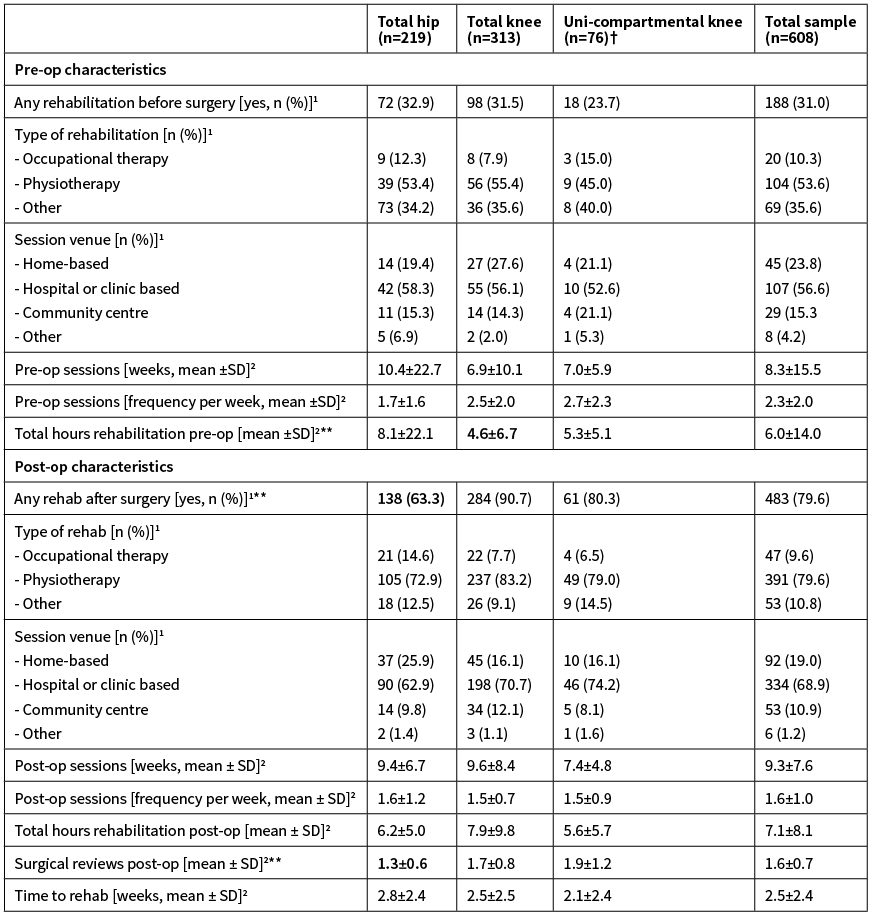
**p<0.05 using non parametric tests (1 = Chi square; 2 = Kruskall-Wallis tests). †Bootstrapping not done because of small sample size.Where significant, data in bold delineates where the difference lies.
There were no differences by procedure type regarding the intensity, location or duration of rehabilitation pre-operatively. Post-operatively, total hip replacement patients were less likely to use rehabilitation than those after total knee or a uni-compartmental knee replacement (total hip: 63.3%, total knee: 90.7%, uni-knee: 80.3%; X2(2)=59.5, p<0.01). There were no differences in the intensity, location or duration of rehabilitation used, but participants undergoing total hip replacement had fewer follow-up appointments with the surgeon than both knee replacement groups (mean number of surgeon visits post-surgery: total hip 1.5; total knee 1.9; uni-knee 1.9; X2(2)=16.86, p<0.01). Finally, use of rehabilitation pre- and post-operatively were highly correlated. Participants who used rehabilitation pre-operatively were more likely to have used rehabilitation post-operatively. Intensity of pre- and post-operative rehabilitation were also correlated in terms of number of hours, session duration, sessions per week and total hours of rehabilitation (total hours: r=0.34, p<0.01; session length: r=0.43, p<0.01; no of weeks of intervention: r=0.29, p<0.01; frequency of sessions per week: r=0.36, p<0.01).
Ethnicity and geographical location
There were no significant differences in use of rehabilitation pre- or post-operatively on the basis of ethnicity. However, nearly 90% of the sample was of New Zealand European ethnicity, with New Zealand Māori making up just 5.5%. The low numbers of non-New Zealand European participants prevented meaningful evaluation of these associations.
Although regional differences in access to surgery were suggested (data not shown), there were no significant differences in use of rehabilitation on the basis of geographical location when this was examined for the full sample. When this was broken down by procedure type the analyses suggested participants undergoing total hip replacement used more pre-operative rehabilitation if they lived in an urban area (60.6%) compared with those living in more rural areas (26.8%; X2 (2)=6.73, p=0.04). There were no other significant associations between access to rehabilitation by geographical region.
Discussion
We characterised patterns of rehabilitation before and after hip and knee replacement and found differences in use of rehabilitation on the basis of procedure type and to a lesser extent, geography. More pre-operative rehabilitation was used by total hip and knee replacement participants compared with uni-compartmental knee replacement participants. Post-operatively those undergoing total hip replacement used less rehabilitation than the other two groups. There is a large body of evidence indicating those undergoing total knee replacements have slower recoveries with ongoing pain and functional impairment within the first 6–12 months compared with other joint replacement groups.4–6,28 Thus it is perhaps unsurprising that total knee participants used more rehabilitation. Our participants predominantly used clinic-based physiotherapy both pre- and post-operatively in keeping with findings in international literature.7,8 Other rehabilitation settings were used less frequently in our sample.
There were trends toward greater use of pre-operative rehabilitation by participants living in larger urban areas, most evident for those undergoing total hip replacement and to a lesser extent for those undergoing uni-compartmental knee replacement. We did not find any other differences in use of rehabilitation on the basis of geography. However, we noticed that a high proportion of participants in our sample live in rural New Zealand or in large urban areas, rather than smaller urban centres. The relationships between use of healthcare services and geography are understudied and depend on the ways these concepts are defined.29 We speculated, based on experiences of the research team, that people living in rural New Zealand may be more willing to travel to access health services. A percentage of people living in smaller towns adjacent to large urban centres may also use urban health services, although this may depend on the way smaller towns are defined or their location.29 The way geographical location was managed in the present study may have been too simplistic to capture such complexities in the joint replacement population.
Clinical and research implications
In the absence of data, it is unclear whether low ethnic diversity in our sample reflects poor uptake of joint replacement and use of rehabilitation among minority groups or a systematic response bias to completion of our survey. Potential inequities on the basis of ethnicity and geography may exist in the joint replacement population. Participants responding to our survey were predominantly New Zealand European and rates across ethnicity categories were inconsistent with general New Zealand population statistics.16,30 Māori make up approximately 15% of New Zealand’s population, however just over 5% of participants identified as Māori in the ROR study sample. Given our recruitment and sampling frame, we are not able to determine whether lack of diversity in our sample reflected lower rates of access to joint replacement and/or use of rehabilitation among non-European groups or low rates of participation in health research. A first step towards resolving this issue would be for the NZJR to routinely report ethnicity information given that the Registry captures more than 95% of all joint replacement surgeries in New Zealand. This may provide helpful baseline information to motivate strategies to address any potential disparities. In addition, development of partnerships with Māori researchers and the Māori community, and more intentional recruitment strategies, may help to bridge the gap between Māori and non-Māori participation in health research.31
The ROR study also highlighted the predominance of rehabilitation provided via outpatient clinics. Such settings may inadvertently create geographic and socioeconomic barriers for access to rehabilitation, for example meeting transport costs and therapy surcharges. Services might consider increasing opportunities for home and community-based rehabilitation. There is mounting evidence that there is little difference in outcomes on the basis of setting10,11,32,33 but broadening options for accessing rehabilitation resources may have considerable benefits, especially for marginalised and minority groups. Other methods and venues, including telemedicine and community outreach have been debated as a means of improving equitable access to health resources more generally.19
Limitations
This study has limitations. One limitation is the representativeness of study participants. We were not able to analyse differences between responders and non-responders to determine this. The NZJR captures more than 95% of joint replacements in New Zealand27 but only samples 20% of this larger group for follow-up collection of patient-reported outcome data. We sampled an even smaller proportion of this 20% taking into account NZJR response rates. However, when we considered demographic and clinical features of the wider NZJR population, our sample is similar across variables such as age, gender, comorbidity levels and procedure type.
It is possible that our sampling method resulted in systematic bias relating to participation in rehabilitation research. Most importantly, our sample may under-represent the experiences of certain subsections of our target population, for example ethnic minority groups, and over-represent the views of those predisposed to do well. We were also not able to determine whether use of rehabilitation was associated with needs or function, or to determine if rehabilitation use described by participants matched that available by health services. Additionally, we asked participants to recall details regarding use of rehabilitation extending back many months and this raises a concern about recall bias. Nonetheless, this analysis drew on the experiences of 608 participants, which makes this one of the larger joint replacement rehabilitation studies. Future research evaluating rehabilitation before and after joint replacement using prospective methods is recommended to address these concerns.
Finally, we did not examine associations between use of rehabilitation and outcomes in this study as our objective was first to describe the landscape of rehabilitation use in the joint replacement population in New Zealand. More robust prospective methods would be recommended for confident examination of associations between these variables.
Conclusions
In this study participants reported generally positive outcomes six months after primary total hip, knee and uni-compartmental knee replacement consistent with the wider literature describing joint replacement outcomes. However, differences in use of rehabilitation were evident depending on procedure type and delays in starting rehabilitation were suggested. Our data also suggest that broadening setting options for rehabilitation before and after joint replacement by increasing use of home and community-based options, and other approaches such as telemedicine, could improve access to rehabilitation resources.
See more related
Aim
Our objective was to describe rehabilitation used before and after joint replacement in New Zealand and evaluate variation based on geography and ethnicity.
Methods
In this descriptive cross-sectional questionnaire-based study we recruited participants 45 years or older (n=608) from the New Zealand Joint Registry six months after primary total hip, total knee or uni-compartmental knee replacement.
Results
The cohort was predominantly New Zealand European (89.9%). The average age of participants was 68.2 years. Less rehabilitation was used pre-operatively (31.0%) than post-operatively (79.6%) and total hip replacement participants reported using less rehabilitation (63.3%) than those after total knee (90.7%) or uni-compartmental knee (80.3%) replacement (p<0.01). There were trends towards more pre-operative rehabilitation for participants living in larger urban areas, most evident for total hip replacement (p<0.05).
Conclusion
Participants reported generally positive outcomes six months after primary total hip, knee and uni-compartmental knee replacement. However, differences in use of rehabilitation services before and after joint replacement were evident depending on joint replaced. Broadening setting options for rehabilitation might improve use of rehabilitation resources.
Authors
Deborah L Snell, Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch; K Anne Sinnott Jerram, Burwood Academy of Independent Living (BAIL), Burwood Hospital, Christchurch; Jennifer A Dunn, Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch; C Jean Hsieh, MedStar Health Research Institute, Hyattsville MD, USA; MedStar National Rehabilitation Hospital, Washington, DC, USA; Gerben DeJong, Department of Rehabilitation Medicine, Georgetown University School of Medicine, Washington DC, USA; MedStar National Rehabilitation Hospital, Washington, DC, USA; Gary J Hooper, Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch.Acknowledgements
This research was supported by a Project Grant from the Canterbury Medical Research Foundation (Grant no 14/07). The authors would like to thank our research assistant, Caroline Norris for her assistance with recruitment and data collection. We acknowledge and thank the staff at the New Zealand Joint Registry who assisted with recruitment and provision of additional data. We also acknowledge the Burwood Academy of Independent Living (BAIL) for hosting the research grant.Correspondence
Dr Deborah Snell, Department of Orthopaedic Surgery and Musculoskeletal Medicine, University of Otago, Christchurch.Correspondence email
debbie.snell@otago.ac.nzCompeting interests
Dr Snell reports grants from Canterbury Medical Research Foundation during the conduct of the study.1. Bischoff-Ferrari H, Lingard E, Losina E, Baron J, Roos E, Phillips C, Mahomed N, Barret J, JP K. Psychosocial and geriatric correlates of functional status after total hip replacement. Arthritis and Rheumatism - Arthritis Care and Research 2004; 51:829–835.
2. Lavernia C, Alcerro J, Brooks L, M R. Mental health and outcomes in primary total joint arthroplasty. Journal of Arthroplasty 2012; 27:1276–1282.
3. Collins N, Roos E. Patient reported outcomes for total hip and knee arthroplasty: Commonly used instruments and attributes of a “good” measure. Clinics in Geriatric Medicine 2012; 28:367–394.
4. Westby MD. Rehabilitation and total joint arthroplasty. Clin Geriatr Med 2012; 28:489–508.
5. Liddle A, Pandit H, Judge A, Murray D. Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Journal of Bone & Joint Surgery 2015; 97:793e801.
6. Lombardi A, Berend K, Walter C, Aziz-Jacobo J, Cheney N. Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clinical Orthopaedics and Related Research 2009; 467:1450e1457.
7. Di Monaco M, Castiglioni C. Which type of exercise therapy is effective after hip arthroplasty? A systematic review of randomized controlled trials. European Journal of Physical and Rehabilitation Medicine 2013; 49:893–907.
8. Artz N, Elvers KT, Lowe CM, Sackley C, Jepson P, Beswick AD. Effectiveness of physiotherapy exercise following total knee replacement: systematic review and meta-analysis. BMC Musculoskelet Disord 2015; 16:15.
9. World Health Organization (WHO) (2017). Rehabilitation in health systems: Geneva Switzerland.
10. Coulter CL, Scarvell JM, Neeman TM, Smith PN. Physiotherapist-directed rehabilitation exercises in the outpatient or home setting improve strength, gait speed and cadence after elective total hip replacement: a systematic review. Journal of Physiotherapy 2013; 59:219–226.
11. Snell D, Hipango J, Sinnott K, Dunn J, Rothwell A, Hsieh C, DeJong G, Hooper G. Rehabilitation after total joint replacement: A scoping study. Disability and Rehabilitation Published online: 23 Mar 2017:1–4.
12. Gill SD, McBurney H. Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil 2013; 94:164–176.
13. Medical Advisory Secretariat (2005). Physiotherapy rehabilitation after total knee or hip replacement: an evidence-based analysis. In: Ontario Health Technology Assessment Series. Care, M.o.H.a.L.-T. (ed): Toronto, Ontario Canada.
14. DeJong G, Tian W, Smout R, Horn S, Putman K, Hsieh C-H, Gassaway J, Smith P. Long-term outcomes of joint replacement rehabilitation patients discharged from skilled nursing and inpatient facilities. Archives of Physical Medicine and Rehabilitation 2009; 90:1306–1316.
15. DeJong G, Horn S, Smout R, Tian W, Putman K, Gassaway J. Joint Replacement Rehabilitation Outcomes upon Discharge from Skilled Nursing Facilities and Inpatient Rehabilitation Facilities. Archives of Physical Medicine & Rehabilitation 2009; 90:1284–1296.
16. Hooper G, Alex A, Rothwell A, Frampton C. Current trends and projections in the utilisation rates of hip and knee replacement in New Zealand from 2001 to 2026. New Zealand Medical Journal 2014; 127.
17. Singleton N, Buddicom E, Vane A, Poutawera V. Are there differences between Maori and non-Maori patients undergoing primary total hip and knee arthroplasty surgery in New Zealand? A registry-based cohort study. New Zealand Medical Journal 2013; 126:23–30.
18. Sheridan N, Kenealy T, Connolly M, Mahony F, Barber A, Boyd M, Carswell P, Clinton J, Devlin G, Doughty R, Dyall L, Kerse N, Kolbe J, Lawrenson R, Moffitt A. Health equity in the New Zealand health care system: a national survey. International Journal for Equity in Health 2011; 10:45–59.
19. Espiner G. Dr Lance O’Sullivan: New Zealander of the Year 2014. In: The New Zealand Listener 2014.
20. Snell D, Sinnott K, Dunn J, Hsieh C-H, De Jong G, Hooper G. Associations between rehabilitation and outcomes after hip and knee replacement: A national survey. Under review 2019.
21. Dripps R. New classification of physical status. Anesthesiology 1963; 24:111.
22. Dawson J, Fitzpatrick R, Carr A. Questionnaire on the perceptions of patients about total hip replacement. Journal of Bone Joint Surgery 1996; 78B:185–190.
23. Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. Journal of Bone Joint Surgery 1998; 80:863–869.
24. Skevington S, Lofty M, O’Connell K. The World Health Organisation’s WHOQOL-Bref quality of life assessment: Psychometric properties and results of the international field trial. A report from the WHOQOL group. Quality of Life Research 2004; 13:299–310.
25. Snell D, Siegert R, Hooper G, Dunn J, Surgenor L. Evaluating quality of life outcomes following joint replacement: validation of a short form of the WHOQOL-Bref. Quality of Life Research 2016; 25:51–61.
26. IBM Corporation (2016). BM SPSS Statistics for Mac, Version 24.0,. IBM Corp: Armonk, NY.
27. New Zealand Orthopaedic Association (NZOA) (2016). New Zealand Joint Registry: Seventeen Year Report (January 1999 to December 2015): Christchurch, New Zealand
28. Liddle A, Judge A, Pandit H, Murray D. Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. The Lancet 2014; 384:1437–1445.
29. Fearnley D, Lawrenson R, Nixon G. ‘Poorly defined’: unknown unknowns in New Zealand Rural Health. New Zealand Medical Journal 2016; 129:77–81.
30. Statistics New Zealand (2013). 2013 Census. New Zealand Government.
31. Selak V, Crengle S, Elley C, Wadham A, Harwood M, Rafter N, Bullen C, Pillai A, Arroll B, Rodgers A. Recruiting equal numbers of indigenous and non-indigenous participants to a ‘polypill’ randomized trial. International Journal for Equity in Health 2013; 12:44–50.
32. Lopez-Liria R, Padilla-Gongora D, Catalan-Matamoros D, Rocamora-Perez P, Perez-de la Cruz S, Fernandez-Sanchez M. Home-based versus hospital-based rehabilitation program after total knee replacement. Biomed Research International 2015.
33. Monticone M, Ferrante S, Rocca B, Salvaderi S, Fiorentini R, Restelli M, Foti C. Home-Based Functional Exercises Aimed at Managing Kinesiophobia Contribute to Improving Disability and Quality of Life of Patients Undergoing Total Knee Arthroplasty: A Randomized Controlled Trial. Archives of Physical Medicine and Rehabilitation 2013; 94:231–239.
