ARTICLE
Vol. 133 No. 1511 |
The role and measurement of patient activation in the management of long-term conditions in New Zealand
In this article we highlight the nature and utility of a construct called patient activation.
Full article available to subscribers
In this article we highlight the nature and utility of a construct called patient activation. This has been broadly defined as people’s knowledge, skills and confidence to manage their own health and healthcare.1 To date over 500 research studies of patient activation have been published, yet we were able to identify only one New Zealand study.2 We believe that patient activation is an important construct that can be measured and used to advantage in New Zealand studies and clinical practice—particularly for patients with one or more long-term conditions (LTCs). After outlining why the notion of patient activation is highly relevant to the management of LTCs in New Zealand today, we focus on its measurement using the Patient Activation Measure (PAM). First we summarise some of the extensive international literature on the PAM’s reliability and validity, and then report findings from our own study of 544 people with LTCs in the MidCentral DHB region. These findings include information on the PAM’s reliability and validity for New Zealand respondents, including how their level of activation relates to their demographic attributes, their health, and to the quality of their experiences with general practice. Results are presented separately for Māori and non Māori participants to enable us to see how the measure works with different ethnicities in Aotearoa New Zealand.
Why is patient activation relevant to long-term condition management?
People living with long-term conditions (LTCs) are increasingly encouraged to improve their knowledge and understanding of their condition/s and engage in self-management activities in order to maintain or improve their health status and quality of life. Self-management and the self-management support provided by health practitioners are gaining a higher profile due to the ageing population and increased prevalence of comorbidity.3 Limited consultation time due to practitioner shortages and problems in access, particularly in rural locations, means that people themselves are required to step up. In a recent Listener interview,4 Wellington GP Jeff Lowe was quoted as saying “the biggest part of the workforce who need to lift their game are patients themselves—we need them to be self-managing far better. We can equip them with the knowledge, data and advice they need, but we do need patients to take ownership of their own health”.
However, there is ambiguity regarding what self-management actually means, and Van de Velde and colleagues5 conducted a concept analysis in an effort to provide an operational definition and to delineate self-management more clearly. They concluded that “self-management is the intrinsically controlled ability of an active, responsible, informed and autonomous individual to live with the medical, role and emotional consequences of his chronic condition(s) in partnership with his social network and the healthcare provider(s)” (p.10). They further propose that self-management incorporates 10 attributes. These include person-oriented—incorporating active involvement, taking responsibility for the care process and coping under adversity, person-environment-oriented—relating to having correct information, an individual approach, reciprocal relationships with providers and openness to social support, and summarising attributes—describing self-management as a lifelong task requiring personal skills such as problem-solving and decision-making.5
Patient activation encompasses the person’s self-management capabilities and engagement with their own health and healthcare.6 According to Hibbard and Gilburt, patient activation is similar to but different from other constructs that may be related to self-management behaviours, including self-efficacy and readiness to change.7 They describe it as a general concept with a broader application than related concepts that tend to focus on a single behavioural outcome such as smoking cessation. This broader approach is appropriate when considering the varied knowledge, skills and tasks involved in self-management of a range of long-term conditions, especially in different combinations. The relevance of patient activation to LTC management should be evident but its application in research and clinical practice requires that it be measurable. This has been achieved through the Patient Activation Measure (PAM) to which we now turn.
The PAM and international evidence
The PAM is a multi-item, self-report measure completed by an individual. The 22-item PAM was initially developed by Hibbard and colleagues using Rasch analysis.1 This was then abbreviated to the 13-item version now in common use.8 It is a Guttman style measure with statements representing four hierarchical stages: (1) belief in the importance of taking an active role (eg, ‘I am the person responsible for taking care of my health’); (2) confidence and knowledge to act (eg, ‘I know what each of my prescribed medications do’); taking action (eg, ‘I am confident that I can carry out medical treatments I may need to do at home’); and (4) staying the course (eg, ‘I am confident that I can maintain lifestyle changes, like healthy eating and exercising, even during times of stress’). For each statement respondents choose one of five Likert-type response options ranging from ‘disagree strongly’ (1) to ‘agree strongly’ (4), or ‘not applicable’. Insignia Health, the licencing body, provides a spreadsheet to weight responses and convert them into scores on a 0–100 point scale where a higher score represents greater activation. Mean scores in the 50s,9–12 60s13–18 and 70s19 have been reported. Individuals’ scores are used to assign them to one of four activation levels: Level 1 (0–47); Level 2 (47.1–55.1); Level 3 (55.2–72.4) and Level 4 (72.5–100). In nine studies involving primary care patients with one or more LTCs, the percentage of people at Level 1 ranged from 6.8 to 18.5%, at Level 2 from 13.0 to 29.1%, at Level 3 from 22.0 to 39.8% and at Level 4 from 17.2 to 51.0%.12–15,17,18,20–22
Reliability
Internal consistency analyses have generated Cronbach’s alphas ranging from .81 to .88.11,15,18,19,23,24 These alphas are interpretable, as PAM responses are uni-dimensional,8 and are of reassuring magnitude. Test-retest reliability of r=.85 using a one-week test interval has been reported using a sample of 65 people prior to undergoing elective spine surgery.25 This appears acceptable given the presumed stability of activation over short time periods. However, the sample was small and the short timeframe is potentially problematic as earlier responses may have been remembered. A few studies have identified changes in PAM scores within the same sample, over longer time periods and without an intervention,12,14,18 suggesting activation is not a fixed attribute.
Validity
Evidence of construct validity should be supported by finding moderate strength relationships between PAM scores and scores on measures of similar health-related constructs. In this section we consider the relationship between patient activation and two other constructs considered to be similar;7 self-efficacy and readiness-to-change. Research has identified patient activation to be correlated with various types of self-efficacy in people with: heart-failure (r=.71);26 cardiac issues (r=.39);11 multiple sclerosis (r=.50);15 depression (r-.51)27 and spinal problems (r=.65).25 While this is a fairly broad range of correlations, all are in the expected direction and of moderate magnitude. Readiness-to-change with respect to living healthily was measured along with patient activation in a sample of 625 healthcare organisation and airline employees, two-thirds of whom had one or more chronic conditions. Higher PAM scores were found in those who had already made behavioural changes (M=73.9) compared to those with no intention to change their behaviour (M=62.4).16 To assist with interpretation of this finding, a 5 point or greater difference in scores is considered to be of clinical significance with respect to changing outcomes.28
Evidence of validity has also been found in relation to behaviour, with PAM scores used to identify people engaging in specific health behaviours such as seeking and using health information9 and self-care.29 Links have also been made to experiences with health practitioners. Higher PAM scores were associated with: more positive ratings of overall care;21 better communication with providers, more contact beyond office appointments and fewer care coordination problems;30 greater satisfaction with care;13,23 increased involvement in treatment plans;13,23 and perceptions that providers have a good interpersonal style and spend enough time with patients.23
With respect to health, PAM scores are positively associated with self-ratings of general health;9,11 mental health;9,16 lower levels of depression;10,11,17,19,31 better physical health/functioning;10,16,19,26 and better quality of life.17,31
As most studies have been cross-sectional, the relationships between patient activation and health or behavioural variables cannot be interpreted causally. Therefore we cannot be sure whether, for example, activation generates better health or vice versa. However, the predictive validity of patient activation has also been explored and PAM scores have been linked to future changes in ratings of healthcare provision,21 improved medication adherence,27 ambulatory care service utilisation and odds of developing another chronic condition.32 Greene et al6 found that PAM scores predicted healthy behaviours, clinical outcomes and costs two years later, and changes in activation level were associated with health outcomes and costs, in expected directions.
Intervention studies have found that it is possible to modify patient activation and provide information on how to do so. For example Greene and colleagues identified five LTC management strategies that may enhance activation: emphasising patient rather than clinician ownership of health; partnering with patients to create goals and strategies to solve problems; collaborative decision-making about small, realistic steps towards healthier behaviours; provision of frequent follow-up support; and showing that they care about their patients’ well-being.28 Alegria and colleagues demonstrated an improvement in activation, as well as efficacy in patient-physician interactions, following a relatively brief intervention.33 In another intervention study PAM scores were compared before and after attendance at a six-session, condition-specific self-management programme. Mean scores increased from 52.2 to 60.2 with 53.9% improving by >4 points.34
There is growing evidence that PAM scores are associated with certain demographic characteristics. Although the findings are mixed with respect to sex and age, higher scores are consistently found for people with more education9–11,14–16,21,26,32 and higher income.9,10,14,16,24
Overall the PAM appears to be a widely used instrument, with international evidence of reliability and validity. However, it is not known how well the measure works in New Zealand, particularly with respect to our indigenous population, and that is what we consider next.
The PAM in New Zealand
The rest of this paper focuses on measuring patient activation in ‘Talking about Health’, a study of people with LTCs based in MidCentral DHB.35 The study has a longitudinal design but only data from the first of three assessments are used in the analyses reported here.
Method
Following ethics approval from the Health & Disability Ethics Committee (ref. 16/NTA/32) study invitations were sent to all people in the DHB aged 18+ years who had a comprehensive health assessment (CHA) documented during the previous three (Māori/Pasifika) or two (other ethnicities) years (N=2,730). The CHA was part of a LTC package of care meaning that potential participants had at least one LTC and were enrolled with a general practice. Questionnaires were sent out (or made available through SurveyMonkey) on receipt of consent forms. Of the 569 (20.8%) people returning questionnaires, 25 did not have sufficient patient activation data to compute scores and levels, therefore the sample consisted of 544 people with LTCs.
Materials
The questionnaire included measures of patient activation (PAM), overall health, physical and mental health, the effect of LTCs on quality of life, general practice experiences and support provided, and demographics.
Health was measured by a single item general rating of overall health from 1 ‘poor’ to 5 ‘excellent’, and by the physical (GPH) and mental health (GMH) scales of the short form of the Patient-Reported Outcomes Measurement Information System global health questionnaire.36 Each scale consists of four items, some rescaled and reverse coded according to the scale instructions. The scale developers reported good internal consistency (GPH α=.81; GMH α=.86), and construct validity; correlations between the PROMIS and the EQ-5D, a widely used health-related quality of life measure, were r=.82 (GPH) and r=.61 (GMH).36
Effect of LTCs on quality of life was measured with a single rating of ‘how much does having one or more long-term conditions affect your quality of life?’ using a scale ranging from 0 ‘no effect’ to 10 ‘very large effect’. This was reverse coded for analysis so that a higher score represents a more positive result in line with the other variables.
General practice experiences (GPE) were assessed in relation to doctors and nurses separately using nine questions from the New Zealand version of the General Practice Assessment Questionnaire.37 Minor wording changes were made and five additional questions were developed by the study team. The item stem was “when you see the doctor/nurse at your practice, how good are they at …” and items covered various aspects of the consultation including listening, making you feel comfortable during a physical examination, involving you in decisions about your care and spending enough time. Response options ranged from 1 ‘very poor’ to 6 ‘excellent’. Two of the 14 questions (relating to involvement of family/whānau/fanau in decision making and practitioners learning about social support needs) were rated as not applicable by a number of respondents and the total General Practitioner (GPE:GP) and Nurse (GPE:N) scales were consequently calculated allowing two missing responses.
General practice team support was rated with the question “how good is the care and support you get for managing your long term conditions from the doctors and nurses at your general practice?” measured on a 0 ‘not at all good’ to 10 ‘extremely good’ scale.
Demographics included sex, age (measured in 10 year increments), ethnicity (more than one was allowed and anyone identifying as Māori or Māori and one or more ethnicities was coded as Māori) and income adequacy (“how well does your total household income meet your everyday needs for such things as accommodation, food, clothing and other necessities” with response options of ‘not enough’, ‘just enough’, ‘enough’ and ‘more than enough’).
SPSS Statistics 20 was used for analysis. Descriptive statistics were used to describe means and percentages and analysis of variance (ANOVA) was used to test the significance of observed mean differences according to level of activation.
Results
Participant details are provided in Table 1.
Table 1: Demographics for Māori (n=81) and non Māori (n=463) participants.
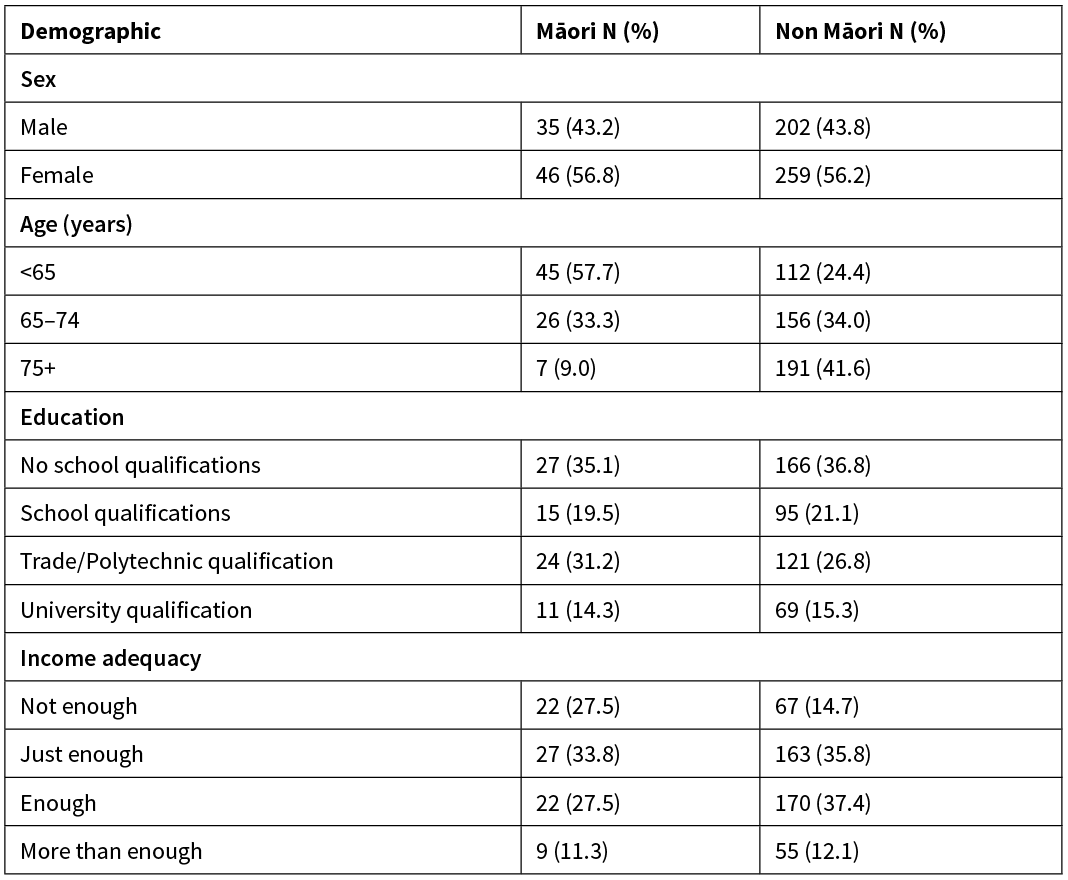
A similar distribution of the sexes and educational level was found for Māori and non Māori. However, Māori participants were younger, in line with the demographic profile for the Māori population and rates of mortality, and reported their income to be less adequate overall.
Descriptive information about PAM scores and levels is provided in Table 2. The score ranges used to define the four levels of activation are reiterated in the table.
Table 2: PAM scores and levels for Māori, non Māori and the total sample.

The mean scores were similar for Māori and non Māori with the main difference being apparent in the percentage of participants at levels 2 and 3. Cronbach’s alphas for PAM scores were .91 for Māori and .90 for non Māori.
To assess construct validity of the PAM with this sample we compared scores on a range of variables considered relevant to people with LTCs within the context of primary LTC care. Mean health and general practice experience scores by patient activation level are presented in Table 3.
Table 3: Mean ratings of health and general practice experiences for Māori and non Māori across different levels of patient activation.
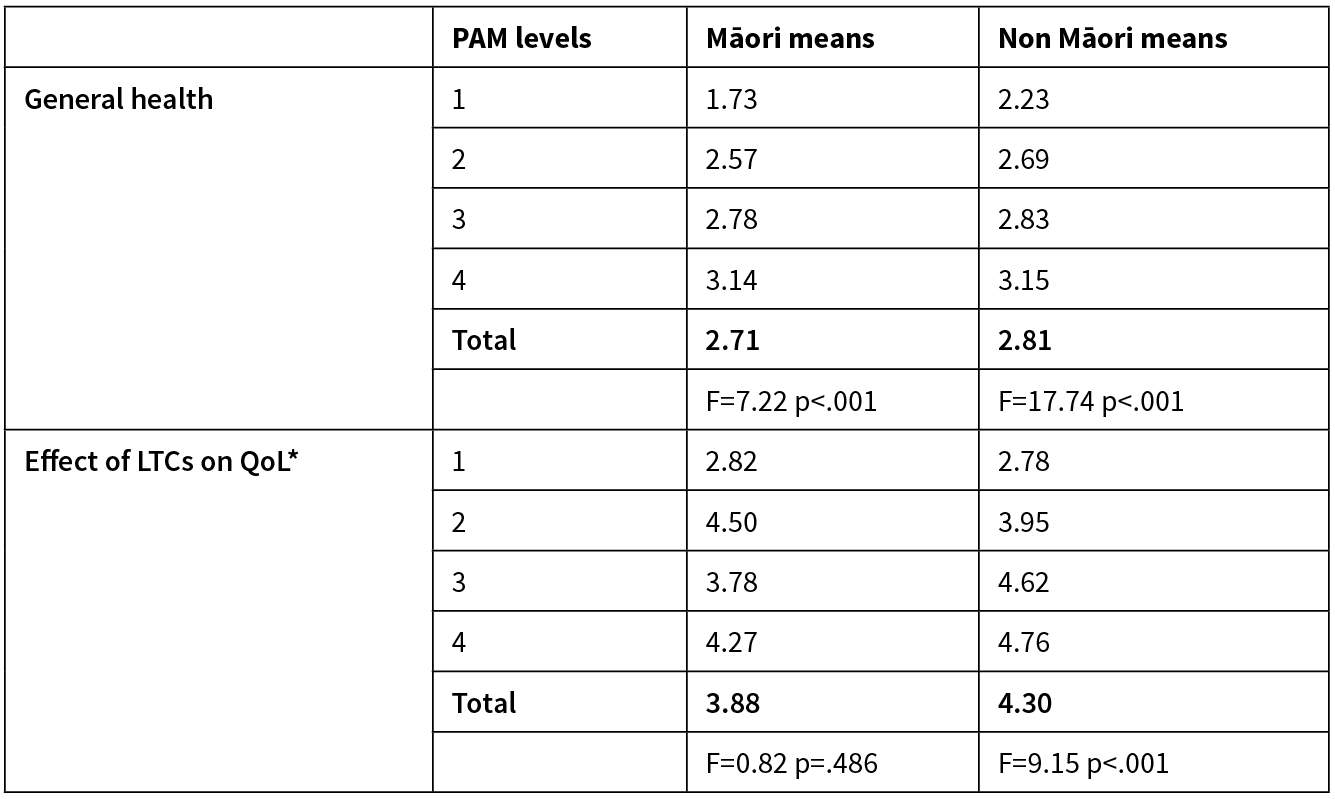

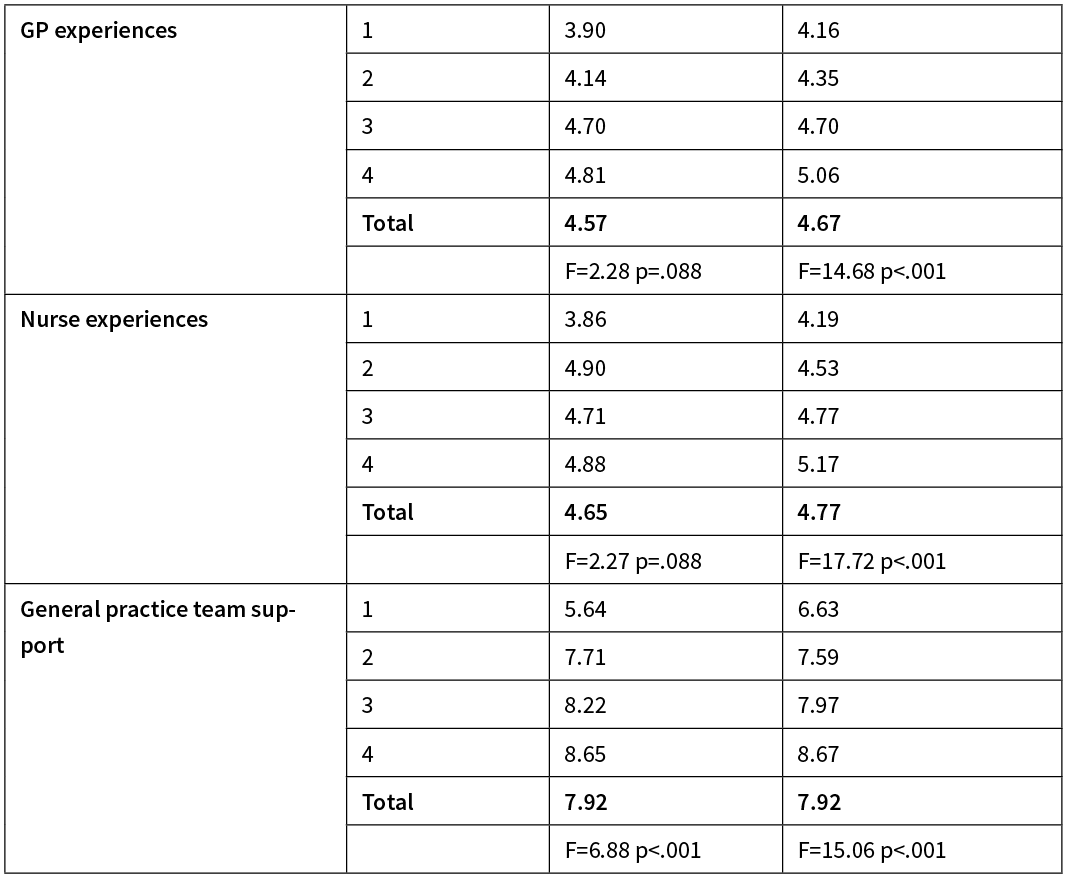
*Reverse coded as described earlier.
The pattern of means in Table 3 is consistent for non Māori and more or less consistent for Māori across these measures; the higher the level of activation, the more positive the ratings of health and general practice experiences and the smaller the perceived effect of long-term conditions on quality of life. Given the large difference in Māori/non Māori sample sizes, the magnitude and pattern of means was of greater interest than the statistical significance of any differences. However, ANOVAs were run to look at the differences in means across levels of activation for Māori and non Māori separately, using Bonferroni adjusted alpha levels of .004 (.05/14). All were significant for non Māori and three were significant for Maori; general health, mental health and GPT support.
Discussion
Self-management, with support from health professionals, whānau and community groups/organisations, is expected of people with long-term conditions. It follows that the more engaged people are in understanding their own conditions, in the decisions made about treatment and in setting realistic goals, the better able they are to have the knowledge and confidence to self-manage on a daily basis. Patient activation appears to represent a set of key attributes of patient engagement and considerable evidence exists to suggest that the measure of patient activation developed by Hibbard and colleagues,8 and comprehensively tested by Hibbard and independent researchers, is reliable, valid and practical.
The patient activation data generated by the Talking about Health study suggests that the measure works similarly for New Zealanders with LTCs as it has in other populations. Overall, mean scores were similar to those found in previous research and the distribution of participants across activation levels was also comparable. The largest proportion of both Māori and non Māori participants were categorised as Level 3 as found in previous studies.9,12,14,15,17,18,20–22,32 With respect to reliability, the level of internal consistency was good for both Māori and non Māori samples with Cronbach’s alphas of .91 and .90 respectively. The pattern of mean scores for health and general practice experiences by activation level indicated that a higher level of activation was associated with more positive ratings of health as well as with higher ratings of experiences with doctors/nurses in the general practice setting and support from general practice teams. This provides evidence of the validity of the measure as well as supporting the results of previous studies described earlier.
Although fewer of the ANOVA results were significant for Māori than non Māori, the difference in sample size may account for this since the range and pattern of means across activation levels was generally similar for both groups. Across the health and general practice measures, the most notable differences in scores were between those at activation Levels 1 and 2. This suggests that the people with the lowest ratings of health and experiences with general practice are also the least activated and are consequently less likely to be able to self-manage well or to adopt behaviours that are challenging or require sustained effort.38 Consequently it is particularly important for these individuals to be identified and receive education and self-management support that is tailored to their level of understanding, current preparedness to engage in a health partnership, and their specific health and social needs. A ‘one size fits all’ approach is clearly not an appropriate way to partner with people with LTCs38 and using a measure such as the PAM is a relatively quick and easy way to identify people’s activation level and undertake risk stratification in order to guide individualised care planning and self-management support. For example, while people at the lower levels may need encouragement to take ownership of their health and contribute more to care planning and identification of personal goals, people at the higher levels can be supported to further their expertise, or to maintain self-management skills in times of major life stress. In this paper we have focused on level of activation, and there is evidence demonstrating changes in health outcomes and costs concomitant with changes in level.6 However the individuals’ PAM scores are also useful for tracking changes over time and for evaluating the impact of interventions as even a small change in the score can be meaningful.28 Regardless of level of activation, a collaborative approach that considers ‘what matters to’ rather than ‘what is the matter with’ the person should be adopted.39
Our study was limited by the small number of Māori participants and further research regarding how well the PAM reflects the Māori worldview would add to our findings and ensure that it is truly has an indigenous application. Other limitations were the convenience sampling, which affected the generalisability of findings, and the use of self-reported data which was consequently prey to the usual biases. However, given how little patient activation research in New Zealand could be found, the current study makes a new contribution to the literature by presenting New Zealand data for Māori and non Māori with LTCs.
More effective long-term condition management is a global priority and given the increasing number of people with long-term conditions, and the rising costs and pressures faced by the health workforce, ways to improve care quality and efficiency are worthy of consideration. The PAM has been adopted by the UK’s National Health System as part of its plan for Universal Personalised Care partly as a risk stratification tool.40 Enhancing patient activation can reduce health inequalities,7 particularly as people at levels 1 and 2 have been shown to be amenable to increases in activation. Consequently, although there are licensing costs associated with using the PAM, we encourage health services in Aotearoa New Zealand to consider this practical way to identify people’s level of engagement with their own health. Services can then be designed, in a culturally appropriate way, to meet the requirements of people at each level of activation with the aim of increasing or maintaining their self-management skills, knowledge and confidence—essential steps to reach the goal for all New Zealanders to “live well, stay well, and get well”.3
Aim
Patient activation represents people’s knowledge, skills and confidence to manage their own health. We provide information regarding the nature of patient activation and use New Zealand data to consider its utility in New Zealand.
Methods
Self-report data using the patient activation measure (PAM) and seven health and general practice experience measures were collected from 544 general practice patients in the MidCentral region. PAM scores were used to categorise respondents into four levels of activation. Mean scores were calculated by activation level, separately for Māori (14.9%) and non Māori (85.1%).
Results
Patterns of activation similar to those reported in earlier research were found. More positive health and general practice experience scores were found for those at higher levels of activation for both ethnicities. The magnitudes of the differences by activation level were similar for both groups and overall differences were significant for all variables for non Māori and for three for Māori.
Conclusion
The PAM behaved as it has done in previous overseas studies with respect to score distribution, reliability and validity. We recommend its use for research and clinical practice in New Zealand to assist with designing appropriate levels of LTC education and self-management support aimed at increasing health engagement.
Authors
Claire Budge, Research Associate, MidCentral DHB, Palmerston North; Melanie Taylor, Project Support Nurse LTC, MidCentral DHB, Palmerston North; Chiquita Hansen, CEO, THINK Hauora, Palmerston North; Folole Fai, Senior Registered Nurse, MidCentral DHB, Palmerston North; Materoa Mar, Upoko Whakarae/Chief Executive, Te Tihi o Ruahine Whānau Ora Alliance and Director of Maori Health, THINK Hauora, Palmerston North.Correspondence
Claire Budge, Research Associate, MidCentral DHB, 33 Old Mill Rd, RD3, Motueka 7198.Correspondence email
clairebudge@gmail.comCompeting interests
Nil.1. Hibbard JH, Stockard J, Mahoney ER, Tussler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004; 39(4):1005–1026.
2. Kersten P, McPherson KM, Kayes NMN, et al. Bridging the goal intention–action gap in rehabilitation: a study of if-then implementation intentions in neurorehabilitation. Disabil Rehabil. 2015; 37(12):1073–1081.
3. Ministry of Health. 2016. Self-management Support for People with Long-term Conditions (2nd ed.). Wellington: Ministry of Health. [Available from: http://www.health.govt.nz/publication/self-management-support-people-long-term-conditions
4. Chisholm D. GP crisis: how the shortage of family doctors is revolutionizing healthcare. NZ Listener. 2019; Aug 10. [Available from: http://www.noted.co.nz/health/health-health/gp-crisis-shortage-family-doctors-is-revolutionising-healthcare
5. Van de Velde D, De Zutter F, Satink T, et al. Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ Open 2019; 9:e027775.
6. Greene J, Hibbard JH, Sacks R, et al. When patient activation levels change, health outcomes and costs change, too. Health Aff. (Milwood) 2015; 34(3):431–437.
7. Hibbard J, Gilburt H. Supporting people to manage their health: An introduction to patient activation. The Kings Fund, 2014. [Available from: http://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/supporting-people-manage-health-patient-activation-may14.pdf
8. Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the Patient Activation Measure. Health Serv Res. 2005; 40(6):1918–1930.
9. Nijman J, Hendriks M, Brabers A, et al. Patient activation and health literacy as predictors of health information use in a general sample of Dutch health care consumers. J Health Commun. 2014; 19(8):955–69.
10. Bos-Touwen I, Schuurmans M, Monninkhof EM, et al. Patient and disease characteristics associated with activation for self-management in patients with diabetes, chronic obstructive pulmonary disease, chronic heart failure and chronic renal disease: a cross-sectional survey study. PLoS ONE; 10(5):e0126400.
11. Ngooi BX, Packer TL, Kephart, G, et al. Validation of the Patient Activation Measure (PAM-13) among adults with cardiac conditions in Singapore. Qual Life Res. 2017; 26(4):1071–1080.
12. Chubak J, Anderson ML, Saunders KW, et al. Predictors of 1-year change in patient activation in older adults with diabetes mellitus and heart disease. J Am Geriatr Soc. 2012; 60:1316–1321.
13. Müllerová H, Landis SH, Aisanov Z. Health behaviors and their correlates among participants in the Continuing to Confront COPD International Patient Survey. Int J Chron Obstruct Pulmon Dis. 2016; 11:881–890.
14. Hibbard JH, Greene J, Shi Y, et al. Taking the long view: how well do patient activation scores predict outcomes four years later? Med Care Res Rev. 2015; 72(3):324–337.
15. Stepleman L, Rutter M-C, Hibbard J, et al. Validation of the patient activation measure in a multiple sclerosis clinic sample and implications for care. Disabil Rehabil. 2010; 32(19):558–1567.
16. Fowles JB, Terry P, Xi M, et al. Measuring self-management of patients’ and employees’ health: Further validation of the Patient Activation Measure (PAM) based on its relation to employee characteristics. Patient Educ Couns. 2009; 77:116–122.
17. Blakemore A, Hann M, Howells K, et al. Patient activation in older people with long-term conditions and multimorbidity: correlates and change in a cohort study in the United Kingdom. BMC Health Serv Res. 2016; 16:582.
18. Rijken M, Heijmans M, Jansen D, et al. Developments in patient activation of people with chronic illness and the impact of changes in self-reported health: results of a nationwide longitudinal study in the Netherlands. Patient Educ Coun. 2014; 97(3):383–390.
19. Smith SG, Curtis LM, Wardle J, et al. Skill set or mind set? Associations between health literacy, patient activation and health. PLoS ONE. 2013; 8(9):e74373.
20. Couture EM, Chouinard M-C, Fortin M, et al. The relationship between health literacy and patient activation among frequent users of healthcare services: a cross sectional study. BMC Fam Pract. 2018; 19(1):38.
21. Aung E, Donald M, Coll JR, et al. Association between patient activation and patient-assessed quality of care in type 2 diabetes: results of a longitudinal study. Health Expect. 2016; 19(2):356–366.
22. Skolasky RL, Frank Green A, Scharfstein D, et al. Psychometric properties of the patient activation measure among multimorbid older adults. Health Serv Res. 2011; 46(2):457–478.
23. Wong ST, Peterson S, Black C. Patient activation in primary care. A comparison between healthier individuals and those with a chronic illness. Med Care. 2011; 49(5):469–479.
24. Lubetkin EI, Wei-Hsin L, Gold, MR. Levels and correlates of patient activation in health center settings: building strategies for improving outcomes. J Health Care Poor Underserved. 2010; 21(3):796–808.
25. Skolasky RL, Mackenzie EJ, Riley III LH, et al. Psychometric properties of the patient activation measure among individuals presenting for elective lumbar spine surgery. Qual Life Res. 2009; 18(10):1357–1366.
26. Young L, Kupzyk K, Barnason S. The impact of self-management knowledge and support on the relationship between self-efficacy, patient activation and self-management in rural heart failure patients. J Cardiovasc Nurs. 2017; 32(4):E1–E8.
27. McCusker J, Lambert SD, Cole MG, et al. Activation and self-efficacy in a randomized trial of a depression self-care intervention. Health Educ Behav. 2016; 43(6):716–725.
28. Greene J, Hibbard JH, Alvarez C, Overton V. Supporting patient behavior change: approaches used by primary care clinicians whose patient have an increase in activation levels. Ann Fam Med. 2016; 14(2):148–154.
29. Hibbard, JH, Tusler M. Assessing activation stage and employing a “next steps” approach to supporting patient self-management. J Ambul Care Manage. 2007; 30(1):2–8.
30. Greene J, Hibbard JH, Sacks R, et al. When seeing the same physician, highly activated patients have better care experiences than less activated patients. Health Aff (Millwood). 2013; 32(7):1299–1306.
31. Magnezi R, Glasser S, Shalev H, et al. Patient activation, depression and quality of life. Patient Educ Couns. 2014; 94:432–437.
32. Hibbard JH, Greene J, Sacks R, et al. Improving population health management strategies: identifying patients who are more likely to be users of avoidable costly care and those more likely to develop a new chronic disease. Health Serv Res. 2017; 52(4):1297–1309.
33. Alegria M, Carson N, Flores M, et al. Activation, self-management, engagement, and retention in behavioral health care: a randomized clinical trial of the DECIDE intervention. JAMA Psychiatry. 2014; 1(5):557–565.
34. Turner A, Anderson JK, Wallace LM, Bourne C. An evaluation of a self-management program for patients with long-term conditions. Patient Educ Coun. 2015; 98:213–219.
35. Taylor M, Budge C, Hansen C, et al. Written care plans and support for health goals: important components of long term conditions care. Kai Tiaki Nursing Research. 2019; 10(1):29–38.
36. Hays RD, Bjorner J, Revicki RA, et al. Development of physical and mental health summary scores from the Patient Reported Outcomes Measurement Information System (PROMIS) global items. Qual Life Res. 2007; 18(7):873–80.
37. Zwier G. A standardised and validated patient survey in primary care: introducing the New Zealand General Practice Assessment Questionnaire (NZGPAQ). NZ Med J. 2013; 126(1372):47–54.
38. Hibbard JH. Using systematic measurement to target consumer activation strategies. Med Care Res Rev. 2009; 66(1):9s–27s.
39. Barry MJ, Edgman-Levitan S. Shared decision making - the pinnacle of patient-centered care. N Engl J Med. 2012; 366(9):780–781.
40. NHS. Patient Activation Measure. http://www.england.nhs.uk/personalisedcare/supported-self-management/patient-activation/
