EDITORIAL
Vol. 134 No. 1546 |
The next phase in Aotearoa New Zealand’s COVID-19 response: a tight suppression strategy may be the best option
In this editorial, we consider the implications of the New Zealand Government’s shift away from a national COVID-19 elimination strategy. This is a critical stage in managing the pandemic.
Full article available to subscribers
In this editorial, we consider the implications of the New Zealand Government’s shift away from a national COVID-19 elimination strategy. This is a critical stage in managing the pandemic, with major uncertainties and difficult trade-offs. We argue that the response should continue to be shaped by key principles: notably, science-informed strategic leadership; a Tiriti and equity focus; use of the precautionary principle; and the need to create legacy benefits for our healthcare and public health systems. These principles support critical actions to get Aotearoa New Zealand through the next phase of the pandemic in the best possible shape from a combined health, equity, wellbeing and economic perspective. These actions include applying a “tight suppression” strategy; rapidly closing the remaining immunity gaps; strengthening public health and social measures, including contact tracing, border management and mask use; and adapting the primary care and hospital system to safely manage large numbers of people presenting with illness from COVID-19.
The elimination phase
The first COVID-19 case was identified in New Zealand in late February 2020, and case numbers rose rapidly in the following month (Figure 1). New Zealand initially followed the mitigation strategy that was core to its influenza pandemic plan.1 A major departure was rapidly switching to an elimination strategy in late March 2020 (Figure 2). Elimination included much stronger border management (quarantine and testing) to prevent importation of cases; testing and contact tracing, so cases could be isolated and contacts quarantined; and an alert level system to guide measures to eliminate community transmission.2,3 The initial, national COVID-19 wave was successfully eliminated by May 2020.4,5 Subsequent outbreaks in Auckland were managed in a similar way, sometimes using rapid, intense circuit-breaker lockdowns to regain elimination.
Accumulating evidence suggests that elimination is probably the optimal initial response to an emerging pandemic disease of moderate or greater severity, at least until vaccines and disease-modifying agents are available.6 The elimination strategy has performed exceptionally well for New Zealand, giving us the lowest COVID-19 mortality in the OECD, a significant increase in life expectancy,7 a relatively high degree of personal freedom for much of the pandemic period and relatively good economic performance.8
The first major upgrade of the elimination strategy was the Reconnecting New Zealanders to the World strategy released on 12 August 2021,9 which proposed a carefully managed increase in inbound travel to New Zealand while continuing with elimination. It implied a more comprehensive revision of the pandemic strategy in early 2022.
Figure 1: Epidemic curve for diagnosed COVID-19 cases in New Zealand, distinguishing cases infected overseas (blue = history of recent overseas travel) from locally acquired cases (red).
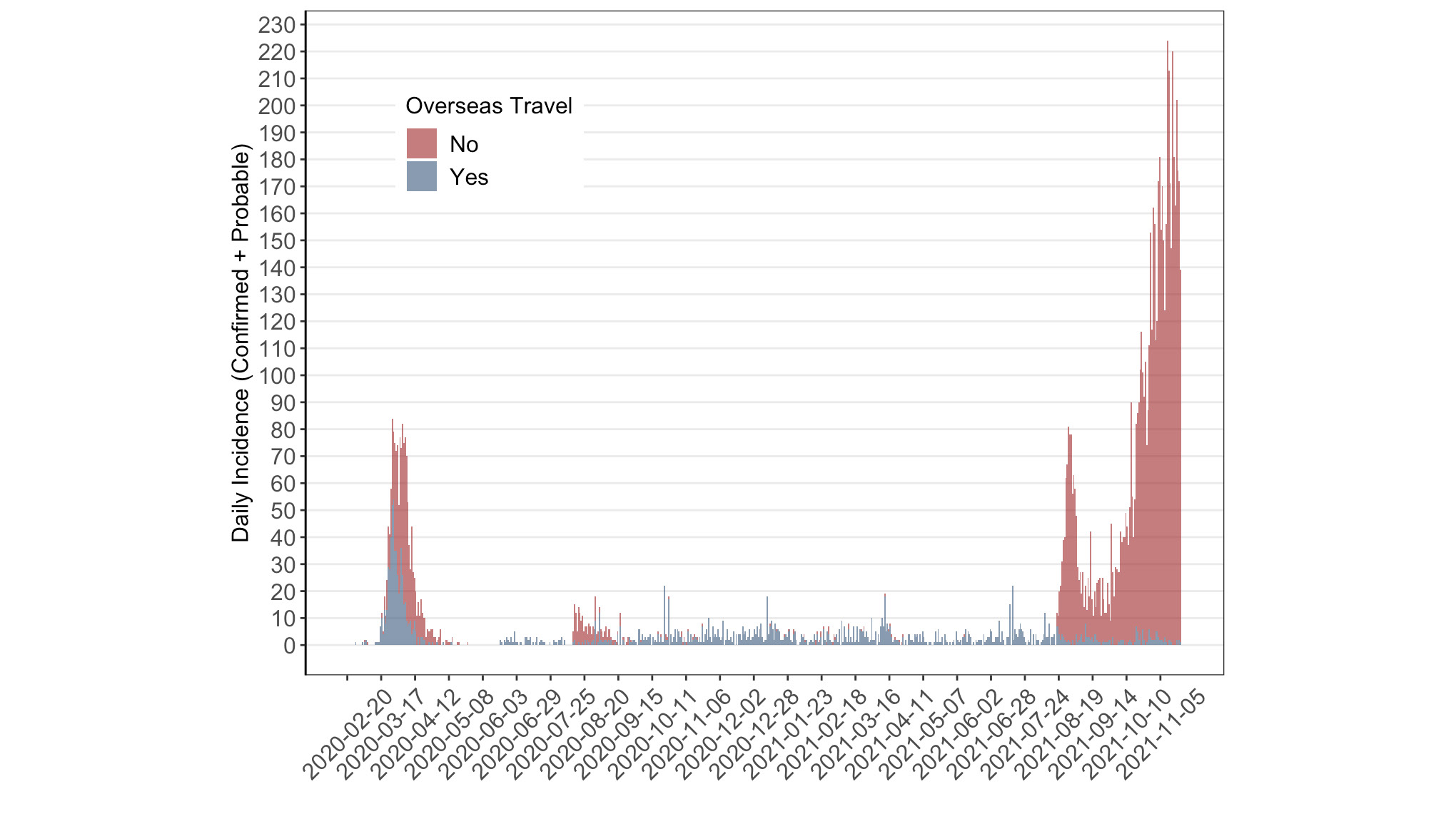
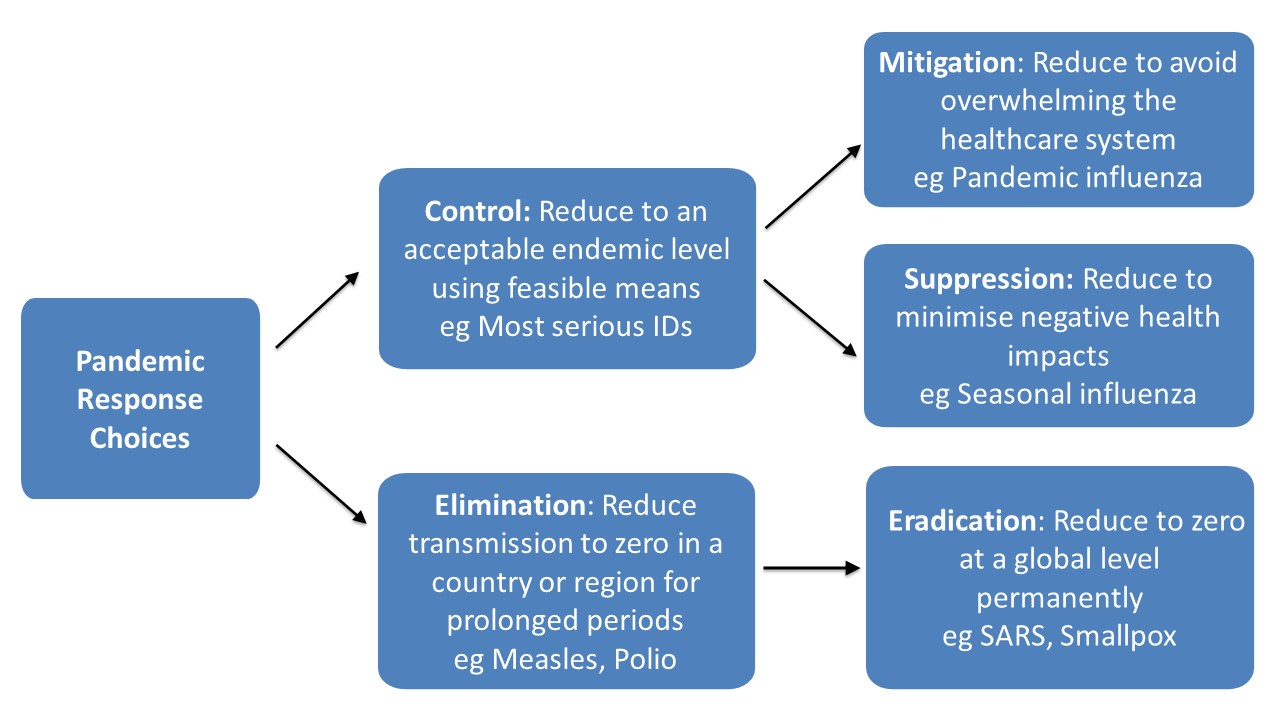
Figure 2: Major strategic choices for managing a pandemic (albeit not including the exclusion strategy successfully used by some Pacific Island nations).
The apparent shift to a suppression strategy
On 4 October 2021, the Prime Minister for the first time indicated New Zealand would transition away from the elimination strategy. The new approach was not formally announced or defined but could be classified as a suppression strategy (Figure 2). This change was precipitated by a Delta-variant outbreak first detected on 17 August 2021 in Auckland (Figure 1). This outbreak proved too difficult to stamp out using the methods that effectively eliminated previous outbreaks arising from border control failures.10
It appears the goal of the new policy settings is to control rather than eliminate SARS-CoV-2 (Figure 2). A positive feature of these settings is that they suggest a “tight suppression” approach, as opposed to loose suppression or mitigation policies used by countries like the United Kingdom and Sweden. Another positive feature is the continuation of many public health and social measures, including restrictions on New Zealand’s external borders and active contact tracing to keep case numbers low. However, there has been little promotion of masks and improvements to indoor ventilation in public spaces, despite the strong evidence base for these measures.11 New Zealand also introduced a range of vaccine mandates for occupational groups and will soon introduce a mandate preventing unvaccinated people from entering a wide range of indoor social settings, such as gyms, restaurants and hairdressers (the COVID-19 Protection Framework, or “traffic light system”).12
At the time of writing, New Zealand is typically experiencing around 150 to 200 new COVID-19 cases a day, mainly in Auckland. Spread from Auckland to other regions has been occurring but at a low level. Consequently, some of us have argued for continuing with suppression in Auckland while maintaining an elimination strategy for the rest New Zealand, which would require maintaining strong boundary controls around Auckland.13
Principles to guide the ongoing pandemic response
There is a series of key principles that can help inform Aotearoa New Zealand’s pandemic response, some of which have been articulated in government plans.14
Science-informed strategic leadership
One of the strongest lessons from the pandemic response comes from the demonstrated benefits of combining effective political and scientific leadership. This success was shown when New Zealand switched its response from the established pandemic mitigation approach to an elimination strategy. Given the ongoing need to meet new challenges in the pandemic response, it would be timely to institutionalise an improved set of processes for decision-making that foster use of evidence, innovation, consensus decision-making, continuous quality improvement and transparency.15,16 These processes could include: convening a cross-party parliamentary group along the lines of the Epidemic Response Committee;17 forming a high-level science strategy rōpū (council) to provide the multidisciplinary expertise needed for complex emergencies; and developing a well-resourced COVID-19 research and development strategy.
Having a Tiriti and equity focus
A major lesson from the pandemic response is the overwhelming importance of health equity. There is a long history of infectious diseases18 and pandemics19 being patterned by inequalities in Aotearoa New Zealand. COVID-19 is unfortunately no exception. Most COVID-19 cases are in Māori and Pacific peoples (71% in the Delta-variant outbreak at the time of writing).20 The markedly lower rates of vaccination in Māori illustrate what happens when Māori input is not adequately sought or ignored, and how long-standing inequities in social determinants drive health outcomes. The lack of engagement with the appropriate people, especially in Auckland, ultimately derailed control efforts and contributed to the current outbreak not being eliminated.21 Key responses need to align with the principles of equity, tino rangatiratanga, partnership and active protection. More fundamentally, there is a need to identify opportunities to strengthen and resource Māori and Pacific leadership of the pandemic response. Creation of the Māori Health Authority will provide a pathway to institutionalise this goal—but this is in the longer term.
Application of the precautionary principle
The precautionary principle expresses the need to take a cautious approach in situations of high uncertainty where decisions have significant impacts,22 such as when infectious diseases like COVID-19 emerge. It is important to recognise and be explicit about these unknowns. We do not know the impact of endemic SARS-CoV-2 infection on morbidity and mortality, even in a highly vaccinated population. An underlying assumption by some appears to be that SARS-CoV-2 infection will inevitably become endemic, and that this infection will be relatively benign once population immunity is widespread, as was eventually seen following the 1918 H1N1 influenza pandemic.23 There is evidence that this assumption may be overly optimistic. The post-acute effects of SARS-CoV-2 infection (so called “long-COVID”) appear to be far more common and severe than for influenza.24 For example, there is the possibility of life-course impacts in the child population through effects on the developing brain.25 If that is found to be the case, then this pathogen may belong in the same category as measles and polio, which create such a burden of illness that they justify efforts for progressive elimination.26 27
One of the biggest unknowns is about the future evolution of SARS-CoV-2 “variants of concern,” which may be more vaccine resistant, more infectious and even more lethal.28 The best way to stem SARS-CoV-2 evolution is to rapidly suppress transmission of this virus to very low levels across the globe, which is technically feasible but difficult to implement given inequities with vaccine supply, public health infrastructure and coordination.
On the positive side, improved vaccines (and vaccine schedules) and disease-modifying treatments are providing tools to reduce both the frequency and consequence of infection. They may even provide the ability to entirely interrupt transmission or make this a trivial infection, or both.
Given this changing landscape, it will be essential to periodically review our strategic direction and policy settings to ensure our response is optimal. It would be unwise to take any option off the table. For example, there may be circumstances in the future where a nationwide return to the elimination strategy, and even global eradication, might become optimal.29
Creating legacy benefits from investment in the response
It is imperative that we gain as many legacy benefits as we can from our huge investment in the pandemic response. We are now almost two years into the pandemic, and it is time to move beyond the crisis phase and establish more mature systems that can undertake robust risk assessment and react swiftly to emerging population health threats. One test is whether the decision-making processes and infrastructure we have developed for this response are sufficiently versatile for future threats, including evolution of the current pandemic and multiple emerging infectious disease threats that require a similarly vigorous response.30,31 The proposed measures in the COVID-19 Protection Framework are not flexible enough to protect New Zealanders against outbreaks of non-COVID infectious diseases (eg, influenza or meningococcal disease) that are likely to occur once border restrictions are loosened and may have atypical epidemiology and severity.31 The time to begin planning and rehearsing for the next pandemic is now.32
The reforms proposed by the new Pae Ora (Healthy Futures) Bill provide an overdue opportunity to create a national public health service that is fit for purpose. Establishing a dedicated national public health agency could consolidate New Zealand’s capacity to deliver a consistently high-quality and sustainable pandemic response, along with other disease prevention and control services across the country and for all its citizens. Such an agency would have an additional valuable role in supporting the pandemic response in the Pacific region. Finally, in the ongoing resource-constrained environment there has never been a better time to Choose Wisely33 for rational and equitable34 healthcare resource stewardship.
Key actions that need to be taken now
Applying these principles supports a number of immediate actions as part of the pandemic response, all of which are underway to varying degrees.
Adopt a tight suppression strategy
We argue that the uncertain public health impacts of the pandemic necessitate a relatively cautious, tight suppression strategy. Tight suppression could extend to elimination outside of Auckland until at least the end of January 2022. This mixed regional approach would increase the time available for the next key action: closing the remaining immunity gaps. A critical decision that will also increase the time available to raise vaccine coverage is careful management of the regional border around Auckland when it “opens” on 15 December, allowing Aucklanders to travel widely across New Zealand. The currently proposed controls will miss many infected people, as they only require vaccination or testing.35 By comparison, even the reduced requirements for travel into New Zealand from overseas that will start in January 2022 still require far more controls (vaccination, pre-travel test, test on arrival, one-week self-isolation, post-isolation test) for a traveller who may have a similar or lower level of risk compared with a traveller from Auckland.36 To maintain even some consistency in risk management, the government needs to set the requirement for travel out of Auckland at a much higher level (a minimum would be full vaccination for those who are eligible plus fully tested for all, including children down to two years of age).
Rapidly close remaining immunity gaps
Disease modelling and international experience indicate that creating and maintaining uniformly high COVID-19 immunity is the most important requirement for minimising the population health impact of COVID-19 with a suppression strategy. New Zealand has extremely low rates of “natural immunity” compared with other countries, so we are very reliant on vaccine-induced immunity. Firstly, we need to achieve high vaccine coverage—that is, as close to 100% as possible for the total population. This is because the dominant Delta variant is highly infectious and, as with previous coronavirus vaccines, the currently available COVID-19 vaccines are not able to create “sterilising immunity” (where people are highly protected from becoming infected and infecting others, as is the case with measles vaccine). Secondly, this coverage needs to be high across all population groups, and protecting those who have a higher risk of infection or adverse outcomes must be a focus. This is not presently the case in New Zealand, where coverage is around 20% lower for Māori (albeit this gap is declining).37 Thirdly, we need to extend coverage to young children. Currently in New Zealand, vaccination is limited to children 12 years of age and older, but several international jurisdictions, including the United States, Canada and Israel, are now vaccinating the 5–11-year age group, with over three million first doses administered. Finally, we need to address waning vaccine immunity over time by providing “booster” doses six months after the first two doses (which may in fact be just part of the primary vaccine course38), and also in future years. These COVID-19 booster doses could potentially be combined with seasonal influenza vaccination.
Strengthen public health and social measures
Although vaccination will certainly reduce case numbers and severity of illness, it is insufficient to prevent all COVID-19 illness. To limit SARS-CoV-2 transmission, we need to continue upgrading our public health and social measures. Many of these measures are familiar from the elimination strategy. However, activation of lockdowns (stay-at-home orders) is less likely with a suppression strategy, where there is a greater tolerance for transmission than there is with elimination. We may need to retain localised lockdowns for situations where cases threaten to overwhelm healthcare services, or if new, more-virulent variants emerge. Effective prevention of transmission in schools requires high uptake of masks and optimising indoor ventilation to prevent spread by inhalation.39–41 It would be useful to develop a nationwide mask strategy to ensure high use of appropriate masks in all settings where this would reduce the risk of SARS-CoV-2 transmission.41 It will also be useful to integrate the use of rapid antigen testing into supporting infection-control actions.42
Strengthen and adapt contact tracing
Testing, contact tracing, case isolation and quarantine of contacts are all essential components of COVID-19 suppression. These measures need to be strengthened so they can manage the potentially large numbers of cases that may arise following the switch from elimination to suppression. The government has recently announcement a new national testing strategy to provide better protection for high-risk groups as New Zealand transitions to the COVID-19 Protection Framework. This strategy will include a new telehealth case investigation service, increased PCR testing capacity and wider use of rapid antigen testing and saliva-based PCR testing.43
Retain border entry controls
Border management is less critical with a suppression strategy in comparison to elimination, and re-designing border controls is now necessary to free-up rooms in MIQ facilities for isolating cases who can’t isolate at home. Nevertheless, border controls will still help reduce the overall case load, especially in regions outside of Auckland. Even the reduced requirements for travel into New Zealand from overseas that will start in January 2022 still require a minimum of full vaccination, multiple tests and one-week self-isolation.36 Tight border management may also need to be reinstated in the future to prevent importation of more virulent SARS-CoV-2 variants.
Strengthen primary healthcare services and support for cases in the community
The primary healthcare system and community support services need to increase their capacity to manage large numbers of people with mild to moderate COVID-19 infection safely in the community.
Strengthen hospital services
The need to assess and manage more seriously ill COVID-19 patients in hospital emergency departments, wards and ICUs will increase. This is a concern, as the healthcare system had limited surge capacity prior to the pandemic, due to heavy demands, resource and workforce constraints. Ultimately, the current healthcare system reform, as outlined in the new Pae Ora (Healthy Futures) Bill, aims to strengthen the capacity and performance of the healthcare system in total.
Ensure effective public communication
The highly effective communication of the elimination strategy was critical to its successful implementation. Since the transition away from elimination was announced on 4 October, and the proposal of the “steps system” and the following “traffic light system,” there has been less clarity and consistency around the pandemic strategy and how it will be achieved. It would be useful to consider ways to ensure clear communication about the current aims of the pandemic strategy and their rationale. Such communication is particularly important for communities where English is a second language, notably some Pacific peoples.
Conclusion
New Zealand’s COVID-19 elimination strategy was highly successful, having maintained positive public health, equity, wellbeing and economic outcomes through the initial phase of the pandemic. The transition away from elimination will be challenging. Outcomes are likely to be optimised by taking a tight suppression approach, minimising immunity gaps and using public health and social measures to protect populations that are more vulnerable to infection and adverse outcomes of infection. All investments in the response should be assessed according to their legacy benefit as well as their immediate value. In this new phase of the response, science-informed strategic leadership and a commitment to equity are more important than ever.
Authors
Michael Baker: Professor of Public Health, Director of CoSearch, Department of Public Health, University of Otago, Wellington. Amanda Kvalsvig: Senior Research Fellow, Co-Director of CoSearch, Department of Public Health, University of Otago Wellington. Sue Crengle: Professor in Māori Health, Department of Preventive and Social Medicine, University of Otago, Dunedin; Specialist General Practitioner, Invercargill. Matire Harwood: Associate Professor, Department of General Practice and Primary Care, University of Auckland; Specialist General Practitioner, Papakura Marae Health Clinic, Auckland. Collin Tukuitonga: Associate Dean (Pacific) and Associate Professor of Public Health, Faculty of Medical and Health Sciences, University of Auckland. Bryan Betty: Medical Director of the Royal New Zealand College of General Practitioners; Specialist General Practitioner, Cannons Creek , East Porirua. John Bonning: FACEM, Emergency Physician Waikato Hospital; Chair of the Council of Medical Colleges of Aotearoa NZ; Immediate Past president ACEM. Nick Wilson: Professor of Public Health, BODE[[3]] Programme, Department of Public Health, University of Otago, Wellington.Acknowledgements
This work was based in the Covid-19 Research Group (CoSearch) at the University of Otago, Wellington which receives funding support from the Health Research Council of NZ (20/1066). The epidemic curve was produced by Andy Anglemyer, Senior Research Fellow, Department of Preventive and Social Medicine, University of Otago, Dunedin.Correspondence
Professor Michael Baker, Department of Public Health, University of Otago, Box 7343, Wellington 6242, New Zealand; 0064 (0)21 355 056Correspondence email
michael.baker@otago.ac.nzCompeting interests
Nil.1. Ministry of Health. New Zealand Influenza Pandemic Plan: A framework for action (2nd edition). Wellington: Ministry of Health, 2017.
2. Baker M, Kvalsvig A, Verrall AJ, et al. New Zealand's elimination strategy for the COVID-19 pandemic and what is required to make it work. N Z Med J. 2020;133(1512):10-4. [published Online First: 2020/04/04]
3. Baker MG, Kvalsvig A, Verrall AJ. New Zealand's COVID-19 elimination strategy. Med J Aust. 2020. doi: 10.5694/mja2.50735 [published Online First: 2020/08/14]
4. Baker MG, Wilson N, Anglemyer A. Successful Elimination of Covid-19 Transmission in New Zealand. N Engl J Med. 2020:e56. doi: 10.1056/NEJMc2025203
5. Jefferies S, French N, Gilkison C, et al. COVID-19 in New Zealand and the impact of the national response: a descriptive epidemiological study. Lancet Public Health. 2020;5(11):e612-e23. doi: 10.1016/S2468-2667(20)30225-5 [published Online First: 2020/10/17]
6. Baker MG, Wilson N, Blakely T. Elimination could be the optimal response strategy for covid-19 and other emerging pandemic diseases. BMJ. 2020;371:m4907. doi: 10.1136/bmj.m4907 [published Online First: 2021/02/10]
7. Islam N, Jdanov DA, Shkolnikov VM, et al. Effects of covid-19 pandemic on life expectancy and premature mortality in 2020: time series analysis in 37 countries. BMJ. 2021;375:e066768. doi: 10.1136/bmj-2021-066768
8. König M, Winkler A. The impact of government responses to the COVID-19 pandemic on GDP growth: Does strategy matter? PLoS ONE. 2021;16(11):e0259362. doi: 10.1371/journal.pone.0259362
9. New Zealand Government [Internet]. The Reconnecting New Zealanders to the World forum 2021. Available from: https://covid19.govt.nz/travel/reconnecting-new-zealand-to-the-world/the-reconnecting-new-zealanders-to-the-world-forum/
10. Grout L, Katar A, Ait Ouakrim D, et al. Failures of quarantine systems for preventing COVID-19 outbreaks in Australia and New Zealand. Med J Aust. 2021;215(7):320-4. doi: 10.5694/mja2.51240 [published Online First: 2021/09/03]
11. Talic S, Shah S, Wild H, et al. Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis. BMJ. 2021;375:e068302. doi: 10.1136/bmj-2021-068302
12. New Zealand Government [Internet]. COVID-19 Protection Framework 2021. Available from: https://covid19.govt.nz/alert-levels-and-updates/covid-19-protection/
13. Wilson N, Summers J, Baker M. The Need for an Updated Strategic Approach to Covid-19 Control in Aotearoa NZ. Public Health Expert (Blog) 2021;9 October. Available from: https://blogs.otago.ac.nz/pubhealthexpert/the-need-for-an-updated-strategic-approach-to-covid-19-control-in-aotearoa-nz/.
14. Ministry of Health [Internet]. COVID-19: Response planning Wellington: Ministry of Health; 2021. Available from: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-response-planning
15. Baker M, Kvalsvig A, Wilson N. 6 months after New Zealand’s first COVID-19 case, it’s time for a more strategic approach. The Conversation, 2020.
16. Baker M, Kvalsvig A, Wilson N. A year on from the arrival of COVID-19 in NZ: 5 lessons for 2021 and beyond. The Conversation, 2020.
17. The New Zealand Parliament [Internet]. Epidemic Response Committee: Covid-19 2020 Wellington 2020. Available from: https://www.parliament.nz/en/visit-and-learn/history-and-buildings/special-topics/epidemic-response-committee-covid-19-2020/
18. Baker MG, Telfar Barnard L, Kvalsvig A, et al. Increasing incidence of serious infectious diseases and inequalities in New Zealand: a national epidemiological study. Lancet. 2012;379(9821):1112-9. doi: 10.1016/s0140-6736(11)61780-7 [published Online First: 2012/02/23]
19. Wilson N, Telfar Barnard L, Summers J, et al. Differential mortality by ethnicity in 3 influenza pandemics over a century, New Zealand. Emerg Infect Dis. 2012;18:71-7. Available from: https://wwwnc.cdc.gov/eid/article/18/1/11-0035_article.
20. Ministry of Health [Internet]. COVID-19: Current cases 2021. Available from: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-data-and-statistics/covid-19-current-cases.
21. Baker M, Crengle S, Tukuitonga C, et al. Five actions to support New Zealand’s Covid-19 response, with a focus on Auckland. Public Health Expert (Blog) 2021;3 October.
22. Kriebel D, Tickner J, Epstein P, et al. The precautionary principle in environmental science. Environ Health Perspect. 2001;109(9):871-6. doi: 10.1289/ehp.01109871
23. Telenti A, Arvin A, Corey L, et al. After the pandemic: perspectives on the future trajectory of COVID-19. Nature 2021;596(7873):495-504. doi: 10.1038/s41586-021-03792-w
24. Taquet M, Dercon Q, Luciano S, et al. Incidence, co-occurrence, and evolution of long-COVID features: A 6-month retrospective cohort study of 273,618 survivors of COVID-19. PLoS Med. 2021;18(9):e1003773. doi: 10.1371/journal.pmed.1003773 [published Online First: 2021/09/29]
25. Baig AM. Counting the neurological cost of COVID-19. Nat Rev Neurol. 2021. doi: 10.1038/s41582-021-00593-7
26. Thompson KM. Modeling and Managing Poliovirus Risks: We are Where we are. Risk Anal. 2021. doi: 10.1111/risa.13668
27. Moss WJ, Griffin DE. Global measles elimination. Nat Rev Microbiol. 2006;4(12):900-8. doi: 10.1038/nrmicro1550
28. Krause PR, Fleming TR, Longini IM, et al. SARS-CoV-2 Variants and Vaccines. N Engl J Med. 2021;385(2):179-86. doi: 10.1056/NEJMsr2105280
29. Wilson N, Mansoor OD, Boyd MJ, et al. We should not dismiss the possibility of eradicating COVID-19: comparisons with smallpox and polio. BMJ Glob Health. 2021;6(8):e006810. doi: 10.1136/bmjgh-2021-006810
30. Boyd M, Baker MG, Wilson N. Border closure for island nations? Analysis of pandemic and bioweapon-related threats suggests some scenarios warrant drastic action. Aust N Z J Public Health. 2020;44(2):89-91. doi: 10.1111/1753-6405.12991 [published Online First: 2020/04/08]
31. Kvalsvig A, Wilson N, Davies C, et al. Expansion of a national Covid-19 alert level system to improve population health and uphold the values of Indigenous peoples. Lancet Reg Health – West Pac 2021;12. doi: 10.1016/j.lanwpc.2021.100206
32. Kvalsvig A, Baker MG. How Aotearoa New Zealand rapidly revised its Covid-19 response strategy: lessons for the next pandemic plan. Journal of the Royal Society of New Zealand. 2021:1-24.
33. The Health Quality & Safety Commission in New Zealand. [Available from: https://www.hqsc.govt.nz/our-programmes/other-topics/choosing-wisely/].
34. Loring BJ, Ineson S, Sherwood D, Tipene-Leach D. Choosing wisely means choosing equity. NZ Med J. 2019 Jun 7;132(1496):6-8.
35. Auckland boundary to change 15 December 2021 [Available from: https://covid19.govt.nz/alert-levels-and-updates/latest-updates/auckland-boundary-to-change-15-december/].
36. Reconnecting New Zealand – the next steps 2021 [Available from: https://www.beehive.govt.nz/release/reconnecting-new-zealand-%E2%80%93-next-steps].
37. Ministry of Health [Internet]. COVID-19: Vaccine data Wellington: Ministry of Health; 2021. Available from: https://www.health.govt.nz/our-work/diseases-and-conditions/covid-19-novel-coronavirus/covid-19-data-and-statistics/covid-19-vaccine-data#group
38. Barda N, Dagan N, Cohen C, et al. Effectiveness of a third dose of the BNT162b2 mRNA COVID-19 vaccine for preventing severe outcomes in Israel: an observational study. Lancet. doi: 10.1016/S0140-6736(21)02249-2
39. Longley I, Bennett J. Monitoring CO2 indoors for improving ventilation as a Covid-19 control tool. Public Health Expert (Blog). Wellington: University of Otago Wellington, 2021:27 October.
40. Kvalsvig A, Bennett J, Russell J, et al. Improving ventilation in schools: a key protection against Covid-19 outbreaks and an enduring legacy for healthier learning. Public Health Expert (Blog). Wellington: University of Otago Wellington, 2021:10 September.
41. Rimar N, Telfar Barnard L, Kvalsvig A, et al. Making the Most of Masks. Public Health Expert (Blog) 2021;9 September.
42. Summers J, Ussher J, Moreland N, et al. Using Rapid Antigen Tests to Improve COVID-19 Control in Aotearoa NZ. Public Health Expert (Blog) 2021;7 October.
43. COVID-19 Protection Framework supported by new testing and contact tracing strategy. [Available from: https://www.beehive.govt.nz/release/covid-19-protection-framework-supported-new-testing-and-contact-tracing-strategy]
