PROCEEDINGS
Vol. 137 No. 1597 |
Proceedings of the New Zealand Society for the Study of Diabetes Annual Scientific Meeting, 2–4 May 2024, Ōtautahi Christchurch
Full article available to subscribers
The projected prevalence of diabetes mellitus in Aotearoa New Zealand, 2020–2044: an age-period-cohort modelling study
Andrea Teng,1 Jason Gurney,1 James Stanley,1 Jeremy Krebs,2 Ross Lawrenson,3 Chunhuan Lao,3 on behalf of the Cancer and Chronic Conditions (C3) Research Group
1Department of Public Health, University of Otago, Wellington
2Department of Medicine, University of Otago, Wellington
3Te Huataki Waiora School of Health, University of Waikato, Hamilton
BACKGROUND
Rates of diabetes have been increasing in Aotearoa New Zealand by approximately 7% per year and are three times higher among Māori and Pacific peoples than Europeans. The depth of the diabetes epidemic, and the expansive breadth of services required for its management, elevate the need for updated evidence on the projected future burden of this complex disease.
METHODS
We have projected the prevalence of diabetes (type 1 and type 2 combined) out to 2040–2044 using Virtual Diabetes Register data on diabetes prevalence trends (2006 to 2019) by age group, calendar period and birth cohort. We then used age-period-cohort (APC) modelling to project diabetes prevalence from 2020 to 2044 (overall, and by gender and ethnicity).
RESULTS
New Zealand will experience a substantial increase in the absolute numbers of people with prevalent diabetes, rising to more than 500,000 by 2044 (approximately 90% increase from 2015–2019). The age-standardised prevalence rate will increase from 3.9% to 5.0%. Both the rate and number of new cases will increase most dramatically for Pacific peoples, especially Pacific females for whom diabetes prevalence is projected to increase to 17% by 2044.
CONCLUSIONS
Increased numbers of people living with diabetes in New Zealand will be driven both by population growth (including our ageing population) as well as increases in prevalence of diabetes in specific groups. These projected increases are likely to stretch our health system to breaking point, if not beyond; and as such, immediate and bold action is required to stem the tide of diabetes and other obesity-related illnesses.
The DiRECT approach in Aotearoa New Zealand: a randomised controlled trial of total meal replacement for adults with diabetes and a desire to lose weight
Campbell K,1,2,3 Peddie M,2 Mann J,1,3 Camp J,1,3 Ashton N,4 Ma’ia’i K,4 Reynolds AN1,3
1Department of Medicine, University of Otago, Dunedin, Aotearoa New Zealand
2Department of Human Nutrition, University of Otago, Dunedin, Aotearoa New Zealand
3Edgar Diabetes and Obesity Research Centre, Aotearoa New Zealand
4Te Kāika Health, Ōtepoti Dunedin, Aotearoa New Zealand
INTRODUCTION
Te Kāika DiRECT is a 12-month randomised controlled trial conducted within a Māori primary healthcare provider in Ōtepoti Dunedin to assess the efficacy and acceptability of an intensive weight management intervention (DiRECT) for adults with type 2 diabetes (T2D) or prediabetes, obesity and a desire to lose weight.
METHODS
Forty participants were randomised to the DiRECT intervention or dietitian-supported usual care. DiRECT involved 3 months of total diet replacement followed by 9 months of dietitian-supported food reintroduction and weight loss maintenance. All participants received the same number of dietetic consults. The primary outcome was weight change at 3 and 12 months. Glycaemia was assessed via continuous glucose monitoring.
RESULTS
Mean weight loss was 6.1kg (95% CI 2.3–9.6kg) greater in the DiRECT arm compared with dietitian-supported care at 3 months, and 4.0kg (7.9–0.05kg) greater at 12 months. Dietitian-supported usual care participants lost an average of <1 kg at 3 months and 2.2 kg at 12 months. The DiRECT group lost >6 kg at 3 months, which was maintained at 12 months. The DiRECT intervention resulted in an average 14.2% increase in time spent in tight glycaemic range (3.9–7.8mmol/L) at 3 months, and a 6.4% increase at 12 months, equivalent to 3.4 and 1.5 additional hours per day, respectively.
CONCLUSIONS
The DiRECT intervention is an effective weight management strategy in our participants with T2D or prediabetes. A larger-scale study investigating the impacts of DiRECT as an Aotearoa-wider intervention is warranted.
Experiences of intergenerational diabetes in a Māori whānau and a Sāmoan aiga
Brooke Williams,1 James Ropati,2 Christine Barthow,1 Eileen McKinlay3
1University of Otago, Wellington
2Univeristy of Otago, Christchurch
3University of Otago, Dunedin
PURPOSE
Many Māori and Pacific families experience intergenerational diabetes. Little is known about the nature and impact of these experiences on individuals and families or how these experiences influence healthcare needs. This study aimed to explore and understand experiences of Māori and Pacific families burdened with intergenerational diabetes.
METHODS
Two case studies: a Māori whānau (family) and a Sāmoan aiga (family) with intergenerational diabetes. One focus group with each was led by culturally matched medical students supported by experienced researchers. Thematic analysis was used to identify key themes.
RESULTS
Four themes were identified: intergenerational trauma and mental health, understanding diabetes and its consequences, the complexity of diabetes and health management and unmet healthcare needs.
Despite the family history of diabetes, little conversation occurred between generations about this condition and there was limited understanding of diabetes when individuals were first diagnosed. Participants identified many complexities related to diabetes management—particularly around medications and seeking healthcare. Limited consultation times and lack of continuity of healthcare had significant consequences. Additionally, complicated life commitment and the need to address other comorbidities of their own and/or other whānau/aiga enhanced the experienced difficulties of intergenerational diabetes. Poor mental health and intergenerational trauma were also detrimental consequences.
CONCLUSIONS
This preliminary study found intergenerational diabetes significantly impacted all participants, both individually and collectively. These experiences resulted in substantial trauma and burdens, which influenced the way whānau/aiga members managed their own diabetes, and how they supported other whānau/aiga affected by the disease.
Are people with diabetes on an equal footing? 5-year incidence (2017–2021) of diabetes foot disease hospitalisations in Aotearoa New Zealand
Michele Garrett,1,2 Rinki Murphy,1,2,3 Tim Kenealy4
1Department of Medicine, Faculty of Medical and Health Sciences, The University of Auckland
2Te Whatu Ora – Health New Zealand, Te Toka Tumai Auckland
3Te Whatu Ora – Health New Zealand, Counties Manukau
4Department of General Practice and Primary Health Care, The University of Auckland (honorary)
INTRODUCTION
The extent and characteristics of diabetes foot disease (DFD) hospitalisations in Aotearoa New Zealand are largely unknown. Objectives were to identify any differences between Māori and non-Māori in the incidence and outcomes for DFD hospitalisations and investigate associated clinical and socio-demographic factors.
METHODS
A national cohort of people with diabetes ≥16 years, alive at 31 December 2016, New Zealand resident and with no prior DFD hospitalisation was identified using the Virtual Diabetes Register (VDR). National health administrative data were used to estimate the 5-year incidence of first DFD hospitalisations including lower limb amputations using ICD-10 codes. Pre-admission demographics, socio-economic variables, comorbidities, rurality and use of selected health services were also analysed.
RESULTS
The VDR cohort contained 236,871 eligible individuals. There were 11,888 DFD hospitalisations (including 1,850 minor and 709 major amputations) over the 5-year period affecting 180,686 individuals. The 5-year incidence rate for DFD hospitalisations was 1.08 per 100 person years (CI 1.06–1.10). The incidence ratio for DFD hospitalisations was 1.71 (CI 1.64–1.79) for Māori compared with non-Māori, 1.70 (CI 1.64–1.77) for males compared with females. DFD hospitalisations incidence rates increased with age, deprivation, comorbidity score and rurality.
CONCLUSIONS
Disparities in DFD outcomes between Māori and non-Māori highlight the need to identify and address inequities in access to preventative care. The identified clinical and socio-demographic factors associated with DFD hospitalisations emphasise these factors need to be considered in optimising DFD care and prevention services.
Increased risk of cardiometabolic and renal disease for all women diagnosed with gestational diabetes mellitus in New Zealand (2001–2010)—a national retrospective cohort study
Barbara Daly,1 Zhenqiang Wu,1 Lynne Chepulis,2 Janet Rowan3
1The University of Auckland, Auckland, New Zealand
2University of Waikato, Hamilton, New Zealand
3National Women’s Health City Hospital, Auckland, New Zealand
INTRODUCTION
The prevalence of gestational diabetes continues to increase, driven by the obesity epidemic and demographic changes. The aim of this study is to compare cardiometabolic and renal outcomes for all women diagnosed with gestational diabetes between 2001 and 2010 with women without diabetes, 10–20 years following delivery.
METHODS
National maternity, hospital and pharmaceutical databases provided information for all women who gave birth between 1 January 2001 and 31 December 2010 (n=604,398) to compare primary and secondary outcomes until 31 May 2021. Adolescent girls <15 years, women >50 years and women with pre-pregnancy diabetes were excluded. In total 11,459 women were diagnosed with gestational diabetes and 11,447 were matched (for age and year of delivery) with 57,235 unexposed (control) women.
RESULTS
Controlling for ethnicity, women with gestational diabetes were significantly more likely than control women to develop diabetes—adjusted HR (95% CI) 20.06 (18.46−21.79); a first cardiovascular event 2.19 (1.86−2.58); renal disease 6.34 (5.35−7.51), all-cause mortality 1.55 (1.31−1.83) and women dispensed at least two antihypertensive 2.77 (2.66–2.88) or lipid-modifying 5.61 (5.31−5.94) medications following delivery, all p-values <0.0001. The HR (95% CI) was similar for each outcome after controlling for all significant covariates. When time-dependent diabetes was included, cardiovascular events 1.33 (1.10−1.61), p=0.003, and renal disease 2.33 (1.88−2.88), p<0.0001, remained significant but not all-cause mortality.
CONCLUSIONS
Women diagnosed with gestational diabetes have an increased risk of developing diabetes and cardiovascular and renal disease. Long-term follow-up screening and management of cardiometabolic and renal risk factors is crucial.
Risk of renal disease progression in young adults with type 2 diabetes
Kanchana Perera,1 John Baker,2,3 Kalpa Jayanatha,4,5 Karen Pickering,2 Richard Cutfield,2,6 Brandon Orr-Walker,2,3 Gerhard Sundborn,7 Andrew Heroy,8,9 Thomas Arnold,8,9,10 Dahai Yu,11 David Simmons1,12
1School of Medicine, Western Sydney University, Campbelltown, Sydney, New South Wales, Australia
2Diabetes Foundation Aotearoa, Ōtara, New Zealand
3Department of Diabetes and Endocrinology, Counties Manukau Health, Auckland, New Zealand
4Department of Renal Medicine, Middlemore Hospital, Auckland, New Zealand
5School of Medicine, Faculty of Medical & Health Sciences, The University of Auckland, Auckland, New Zealand
6Department of Diabetes and Endocrinology, Waitematā District Health Board, Auckland, New Zealand
7Section of Pacific Health, The University of Auckland, Auckland, New Zealand
8Military Cardiovascular Outcomes Research Program, Uniformed Services University, Maryland, United States of America
9Metis Foundation, 84 NE Interstate Loop 410, Suite 325, San Antonio, TX 78216
10Department of Biostatistics, Brown University, 121 S Main Street, Providence, RI 02903
11Primary Care Centre versus Arthritis, School of Medicine, Keele University, Keele ST5 5BG, UK
12Translational Health Research Institute (THRI), Western Sydney University, Campbelltown, Sydney, New South Wales, Australia
INTRODUCTION
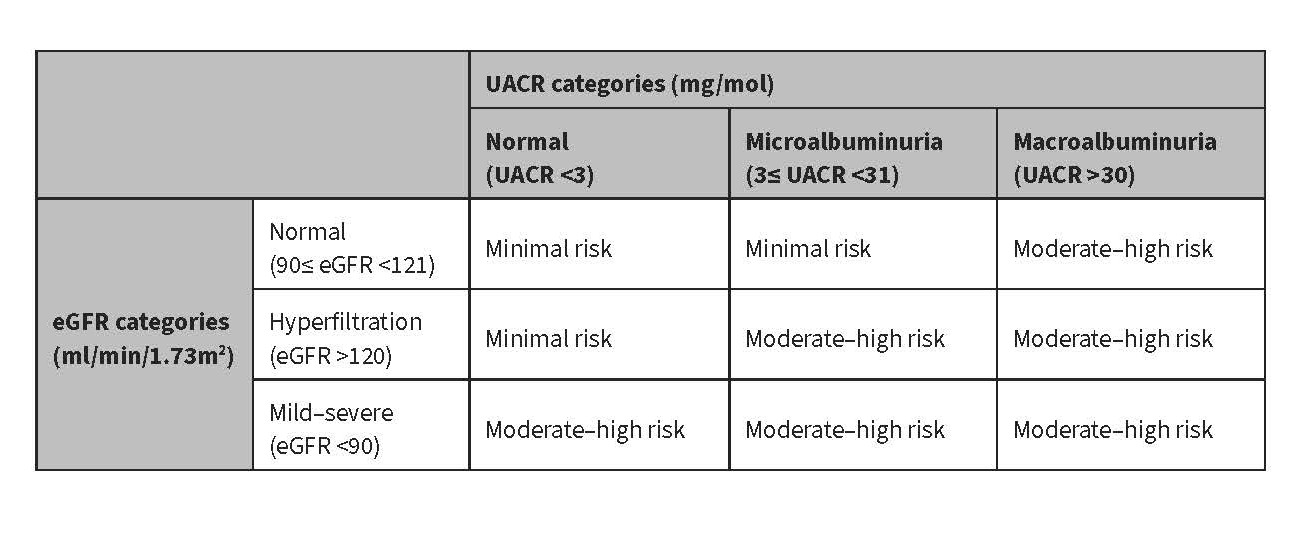
Young adults in New Zealand with type 2 diabetes (T2D) are at high risk of diabetic kidney disease (DKD). This study compared the characteristics of New Zealand European (NZE), Māori, and Pacific young adults (aged 18–40 years) based on a composite urine albumin:creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) variable in order to better stratify DKD progression risk.
METHODS
A secondary analysis of entrants into a longitudinal primary care T2D audit (DCSS:1994–2018). Ethnic comparisons used Chi-squared or ANOVA tests with post hoc Tukey for each DKD risk group defined by the composite UACR/eGFR threshold (see above table).
RESULTS
Of 2,184 young adults, 170 NZE (34.2%), 277 Māori (41.0%) and 481 Pacific (47.5%) were high risk for DKD progression (p<0.001). Compared with NZE, Māori and Pacific at high risk had higher BMI (35.9±8.7 vs 39.3±8.9 and 39.2±8.9kg/m2; p<0.001), lower socio-economic position (21.2% vs 54.5% and 64.9%; p<0.001), and with higher HbA1c (60±22 vs 73±23 and 75±25 mmol/mol; p=0.001). Additionally, they were more likely to receive antihypertensive (67.7% vs 82.3% and 78.8%; p=0.001), anti-diabetes (88.8% vs 94.6% and 93.8%; p=0.047) and anti-lipid medication (62.9% vs 74.7% and 65.1%; p=0.009). Compared with Māori, Pacific had a lower SBP (132.3±17.9 vs 128.6±15.8mmHg; p=0.010) and DBP (84.7±12.3 vs 82.1±10.9mmHg; p=0.007). Current/prior smoking was the most common among Māori (51.6% vs 31.2% (NZE); 37.0% (Pacific); p<0.001).
CONCLUSIONS
Significant ethnic differences exist in socio-demographic and clinical characteristics among young adults with T2D. The use of a composite UACR/eGFR allows for more precise measure of DKD risk than utilising these variables individually.
First in human feasibility study; automated insulin delivery utilising the Dexcom next generation algorithm in adults with type 1 diabetes
Tom Wilkinson,1 Renee Meier,1 Alisa Boucsein,2 Shirley Jones,2 Dave Ballagh,3 Reon van Rensburg,3 Ryan Paul,4 Enrique Composnanez,5 Steve Patek,5 Benjamin Wheeler,2 Martin de Bock2,6
1Department of Paediatrics, University of Otago Christchurch, Christchurch, New Zealand
2Department of Women’s and Children’s Health, University of Otago, Dunedin, New Zealand
3Te Whatu Ora Nelson Marlborough, Blenheim, New Zealand
4He Huataki Waiora School of Health, University of Waikato, Hamilton, New Zealand
5Dexcom Incorporated, San Diego, California, United States of America
6Te Whatu Ora Waitaha, Christchurch, New Zealand
INTRODUCTION
Existing commercial closed-loop systems require pre-meal carbohydrate announcement and are therefore termed “hybrid closed-loop.” This study assessed a novel “fully automated” closed-loop system that does not require carbohydrate announcement, in adults with type 1 diabetes (T1D).
METHODS
Single-arm feasibility study, comprising 14-day run-in using participants’ usual insulin therapy with “blinded” continuous glucose monitoring (CGM), followed by 12 weeks’ use of investigational closed-loop system incorporating an YpsoPump® insulin pump, Dexcom G6 CGM and control algorithm on an Android smartphone. Outcome measures were CGM metrics (run-in and last 14 days of intervention), HbA1c and adverse events.
RESULTS
Thirty-two participants with T1D (mean age 45 years, range 17–74; 17 [53%] female; 4 [13%] Māori; 13 [41%] existing insulin pump users) were enrolled.
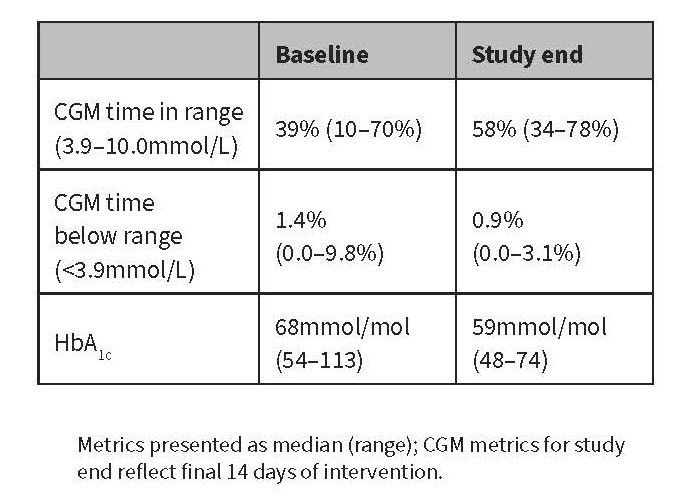
Seven participants withdrew, of whom two were excluded from analysis due to <14 days intervention data. Reasons for withdrawal were severe adverse events in three participants (worsening retinopathy; severe hypoglycaemia attributable to user error; acute hospital admission unrelated to device), and device intolerance in four pump-naïve participants. No other severe adverse events occurred.
CONCLUSIONS
A fully automated closed-loop system, requiring no meal announcement, demonstrated feasibility in a cohort of adults with T1D, with the greatest benefit seen in participants with suboptimal baseline control.
First in human feasibility study; automated insulin delivery utilising the Dexcom next generation algorithm in adults with type 2 diabetes
Solita Donnelly,1 Claire Lever1,2 (Ngāi Tahu), Tom Wilkinson,3 Enrique Composnanez,4 Steve Patek,4 Rachael Sampson,1 Ryan Paul1,2 (Ngāti Maru Hauraki), Martin de Bock3
1Aotearoa Diabetes Collective, Waikato, New Zealand
2Te Huataki Waiora, School of Health, University of Waikato, Hamilton, New Zealand
3Department of Paediatrics, University of Otago Christchurch, Christchurch, New Zealand
4Dexcom Incorporated, San Diego, California, United States of America
INTRODUCTION
Automated insulin delivery technology is under-studied in Indigenous type 2 populations. This study assessed the safety and efficacy of a novel “fully automated” closed-loop system that does not require carbohydrate announcement in Māori and Pacific adults with type 2 diabetes (T2D) and elevated HbA1c.
METHODS
Single-arm feasibility study, with a 14-day run-in period where participants continued their standard insulin therapy with “blinded” continuous glucose monitoring (CGM), followed by up to 12 weeks’ use of the investigational closed-loop system incorporating a YpsoPump® insulin pump, Dexcom G6 CGM and control algorithm installed on an Android smartphone. Outcome measures were CGM metrics, HbA1c and safety data.
RESULTS
Ten Māori and Pacific participants were enrolled; median age 55 (range 39–69) years, 4 (40%) female, median HbA1c 90mmol/mol (range 59–158mmol/mol). All participants completed the study. Median time in range (% CGM recordings 3.9–10.0mmol/L) increased from 10% (range <1–51%) at baseline to 55% (range 2–96%) during the last 14 days of the intervention. Time <3.9mmol/L was <1% during run-in and at end of study. HbA1c was 60 (range 52–117) mmol/mol at study completion. There were no episodes of severe hypoglycaemia or ketoacidosis. Mean (±SD) weight change was +6.2 (4.4) kg.
CONCLUSIONS
A novel fully automated closed-loop system, requiring no carbohydrate announcement, safely improved glycaemic control without increasing time spent in hypoglycaemia in a cohort of Māori and Pacific adults with suboptimally controlled insulin-requiring T2D.
CGMs alongside culturally appropriate wrap-around care significantly improves clinical outcomes and self-management in Māori patients with type 2 diabetes: a mixed methods study
Rebekah Crosswell (Whakatōhea),1 Hamish Crocket,1 Suzanne Moorhouse,2 Donna Foxall (Tainui),1 Helen Morton,3 Michael Oehley,3 Salem Waters (Tainui),1 Ryan Paul (Ngāti Maru—Hauraki),1,4 Lynne Chepulis1
¹Waikato Medical Research Centre, Te Huataki Waiora School of Health, University of Waikato, Hamilton, New Zealand
²Hauraki Primary Healthcare Organisation, Hamilton, New Zealand
³Raukura Hauora o Tainui, Hamilton New Zealand
4Te Whatu Ora Waikato (Health New Zealand), Hamilton, New Zealand
BACKGROUND
In Aotearoa New Zealand, Māori populations are disproportionately affected by type 2 diabetes (T2D) and have higher rates of morbidity and mortality. This pilot study evaluates the use of continuous glucose monitoring (CGM) with culturally relevant education and support in a high-needs Māori population in primary care.
METHODS
Twenty-three participants with HbA1c >80 mmol/L were recruited from Raukura Hauora O Tainui during 2022/2023. The Kaupapa Māori informed study utilised principles of whakawhanaungatanga (relationship building) and manaakitanga (respect/care) alongside awhi (care) and mana (power). Participants received 2–4 weeks of CGM wear at baseline and 3 months, alongside kaiāwhina-based T2D education. Clinical biomarkers and psychometric measures were recorded at 0, 3 and 6 months. Ten qualitative interviews were completed at 4 and/or 12 weeks.
RESULTS
Mean (± SD) HbA1c significantly decreased from 93.4±15.7mmol/mol at baseline to 76.5±14.8mmol/mol at 3 months with reductions maintained at 6 months (both P<0.001 vs baseline). Diabetes self-management scores increased from 4.0±1.5 to 6.2±1.1 (P<0.05) though no other significant reductions were observed. Interviews identified the equal importance of manaakitanga, education and technology use.
CONCLUSIONS
CGM use alongside wrap-around care grounded in Te Ao Māori has the potential to improve T2D primary care and self-management in Māori adults. Further work is required to understand the importance of the different study components (e.g., CGM vs kaiāwhina) and to explore how to embed this model of care into primary care.
In vivo test results for an open-source, Ultra Low Cost insulin pump
Matthew Payne,1 Francis Pooke,1 Tom Wilkinson,2 Bronte Chamberlain,2 Lui Holder-Pearson,1 Martin de Bock,2,3 J Geoffrey Chase1
1Department of Mechanical Engineering, Centre for Bio-engineering, University of Canterbury, New Zealand
2Department of Paediatrics, University of Otago, Christchurch, New Zealand
3Department of Paediatrics, Canterbury District Health Board, Christchurch, New Zealand
BACKGROUND
The high cost of commercial insulin pumps may limit accessibility to people with type 1 diabetes (T1D) who would otherwise benefit, exacerbating inequities in diabetes care. An interoperable, open-source, Ultra Low Cost insulin pump (ULCIP) has shown comparable delivery accuracy to commercial models in laboratory tests. This first-in-human study assessed safety and usability of the ULCIP.
METHODS
Six participants with T1D, usually on insulin pump therapy, used the ULCIP during a supervised 9-hour inpatient stay, including two meals with matched boluses. In addition to continuous glucose monitoring (Dexcom G7), venous blood samples were taken hourly for glucose, β-hydroxybutyrate and insulin.
RESULTS
The ULCIP effectively delivered insulin to five participants, evidenced by glucose and insulin levels displaying trends consistent with programmed pump insulin delivery, and β-hydroxybutyrate consistently <0.6mmol/L. One participant developed mild ketosis; however, they were able to safely resume ULCIP use following treatment and identification of an underlying remediable hardware issue.
CONCLUSION
The ULCIP was able to effectively deliver insulin to participants in an inpatient setting and has potential as a treatment for people with T1D currently unable to access commercial insulin pumps. Further development will address a hardware issue identified in this trial and enhance Bluetooth operability to enable use in closed-loop systems.
Acceptability, enablers and barriers to dietary change for Māori with nutrition-related conditions in Aotearoa New Zealand: a scoping review
Christina McKerchar1 (Ngāti Porou, Ngāti Kahungunu, Tūhoe), Christine Barthow,2 Tania Huria3 (Ngāi Tahu, Ngāti Mutunga o Wharekauri), Bernadette Jones2 (Ngā Wairiki, Ngāti Apa), Kirsten Coppell,2 Rosemary Hall,2 Tutangi Amataiti,2 Amber Parry-Strong,4 Soana Muimuiheata,5 Morag Wright-McNaughton,6 Jeremy Krebs2
1Department of Population Health, University of Otago, Christchurch 8140, PO Box 4345, New Zealand
2Department of Medicine, University of Otago, Wellington South 6242, PO Box 7343, New Zealand
3Department of Māori Indigenous Health Innovation, University of Otago, Christchurch 8140, PO Box 4345, New Zealand
4Centre for Endocrine, Diabetes and Obesity Research (CEDOR), Wellington South, PO Box 7902, New Zealand
5Total Well-being Consultancy Services Ltd, 222b Buckland Road, Mangere East, Auckland 2024, New Zealand
6Formerly of Department of Medicine, University of Otago, Wellington South 6242, PO Box 7343, New Zealand
INTRODUCTION
Māori, the Indigenous population of Aotearoa New Zealand, face a substantial burden of nutrition-related diseases, especially obesity and type 2 diabetes. Weight loss, through dietary change, is a central component of obesity and diabetes prevention and management; however, most approaches have not been designed with or evaluated specifically for Māori. The aim of this study was to review literature on the acceptability, enablers and barriers to dietary change for Māori.
METHODS
Relevant literature published from January 2000 to August 2021 was identified by searches in Medline (Ovid), Embase (Ovid), Scopus, Indigenous health (informit), CINAHL (EBSCO), Web of Science and NZ Research. Studies included Māori and reflected enablers and barriers to dietary change for individuals/whānau (families). Data identifying the aims, methods, interventions, location, population studied and identified enablers and barriers to dietary change and responsiveness to Māori were extracted. Enablers and barriers to dietary change were mapped to a New Zealand Indigenous health framework, the Meihana model.
RESULTS
Twenty-two of 77 identified records met the inclusion criteria. Records included a diverse range of research approaches and most related to mixed ethnic groups rather than solely Māori populations.
CONCLUSIONS
Using a relevant Indigenous model, this study highlights that multiple and diverse enablers and barriers to dietary change exist for Māori. While some are likely common to all populations, this review highlights the critical importance of developing interventions in close partnership with Indigenous communities to mitigate the impacts of colonisation and racism and to be grounded in Indigenous understandings of health.
Dietary fibre more important than carbohydrate amount for adults with diabetes: systematic review and meta-analyses
Andrew N Reynolds,1,2 Jessica Lang,2 Amanda Brand,3 Celeste Naude,3 Jim Mann1,2
1Edgar Diabetes and Obesity Research Centre, University of Otago, Dunedin, New Zealand
2Department of Medicine, University of Otago, Dunedin, New Zealand
3Centre for Evidence-Based Health Care, Division of Epidemiology and Biostatistics, Stellenbosch University, Stellenbosch, South Africa
INTRODUCTION
We have compared the effects on cardiometabolic risk factors of diets higher in both carbohydrate and fibre with lower carbohydrate diets in people with diabetes.
METHODS
Randomised controlled trials in which both carbohydrate amount and dietary fibre had been modified were identified from the existing systematic reviews on carbohydrate amount. Ovid MEDLINE, Embase and the Cochrane Register of Systematic Reviews were searched up to 2 November 2023. We pooled outcomes from the eligible trials with random effects and conducted robust sensitivity analyses. Pooled evidence was graded.
RESULTS
Ten trials including 499 participants with diabetes were identified from the potentially eligible 812 included in existing systematic reviews. Pooled findings indicate that higher carbohydrate, high-fibre diets reduced HbA1c (mean difference [MD] -0.50% [-0.99 to -0.02]), fasting insulin (MD -5.9 pmol/L [-11.0 to -0.9]), total cholesterol (MD -0.16 mmol/L [-0.27 to -0.05]) and LDL cholesterol (MD -0.16 mmol/L [-0.31 to -0.01] when compared with lower carbohydrate diets. Trials with larger differences in carbohydrate and fibre intakes between intervention arms reported greater reductions. Certainty of evidence for these outcomes was moderate to high, with most outcomes downgraded due to heterogeneity unexplained by any single variable.
CONCLUSIONS
Our findings provide further evidence of the importance of promoting dietary fibre intakes, and the relative unimportance of focussing on carbohydrate amount in nutrition recommendations for people with diabetes.
This project was unfunded. Prospective review registration CRD42023473322.
Specialist weight management programme to improve health outcomes in Counties Manukau communities
Soana Muimuiheata,1 Katherine Zhang,1 Emma Smirk,1 James Shand,1 Rinki Murphy1,2
1Te Whatu Ora Counties Manukau, Auckland, New Zealand
2Faculty of Medical and Health Sciences, The University of Auckland, Auckland, New Zealand
INTRODUCTION
In New Zealand there is a high prevalence of obesity and type 2 diabetes, particularly in Māori and Pacific peoples, with very limited secondary care level interventions focussing on intensive weight management besides bariatric surgery. Te Mana Ki Tua (TMKT), a specialist weight management service, was designed to provide an evidence-based model of secondary care incorporating Tiriti principles for intensive weight management, targeting remission of type 2 diabetes and contributing to Ola Manuia outcomes.
METHODS
TMKT is a multidisciplinary team (MDT) programme for people in Counties Manukau. Patients were predominantly type 2 diabetes, with a body mass index (BMI) >35 and low priority for bariatric surgery. Meal replacements (Optifast for first cohort, Counterweight for all subsequent cohorts) were provided for first 20 weeks. Patients attended group and 1:1 support sessions for 1 year with a whānau-based approach addressing equity.
RESULTS
Of 182 (44 Māori, 82 Pacific, 33 European, 16 Asian, 7 other) invited, 64 (12 Māori, 33 Pacific, 14 European, 5 Asian) were enrolled in monthly intakes of 7–15 patients between July 2023 and February 2024. Remission of type 2 diabetes was 42% based on preliminary data at 3 months. Mean weight loss at 3 months is 10.6kg (7.8% body weight). Mean percentage weight loss was strongly correlated with number of group sessions attended. Hua Oranga wellbeing scores improved (data from one group increased from 65.4 to 71.5).
CONCLUSIONS
Early diabetes remission and weight loss results are comparable to that seen at 12 months in United Kingdom in the DiRECT study.
“Piki Te Ora”: a qualitative evaluation of type 2 diabetes self-management model in primary care
Rebekah Crosswell (Whakatōhea),¹ Karis Gordon,¹ Keimarire Tibble-Brown (Ngāti Ranginui, Ngāti Pūkenga ki Manaia, Ngāti Porou, Ngāti Tūwharetoa),¹ Claire Cannon,² Hilde Mullins (Kahungunu ki Wairarapa),³ Donna Foxall (Tainui),³ Lynne Chepulis¹
¹Waikato Medical Research Centre, Te Huataki Waiora School of Health, University of Waikato, Hamilton, New Zealand
²Te Korowai Hauora o Hauraki, Thames, New Zealand
³Department of Nursing, Te Huataki Waiora School of Health, University of Waikato, Hamilton, New Zealand
AIMS AND OBJECTIVES
Type 2 diabetes (T2D) is a chronic condition, yet despite established guidelines for treatment, there is still suboptimal disease management in primary care. Cultural inequities are also prevalent, with a higher proportion of Māori patients having poorer health outcomes. Difficulties in diabetes care have led to the development of alternative models of care to reduce disparities and improve self-management. This qualitative study aimed to explore T2D patients’ experiences of “Piki Te Ora”, a holistic chronic care programme running in primary care.
METHODS
Qualitative semi-structured interviews were completed December–January 2023/2024, involving 10 participants (six female, four male), five of whom were Māori, five NZ European. Recruitment was through a Māori health provider, Te Korowai Hauora o Hauraki, located in the Coromandel/Thames area. Participants were texted a link to opt into a survey (larger study) and then registered their interest by providing their contact details for an in-depth interview (current study). All interviews were audio recorded, transcribed orthographically and thematically analysed.
RESULTS
Four main overarching themes were established including accessibility, support/care (manaakitanga), individualised care and empowerment (whakamana). Patients expressed a preference for the Piki Te Ora programme compared to Westernised mainstream models of care, which they attributed to appointment difficulties (short appointments and long waiting times), financial and travel barriers, discontent with service delivery, transport issues, financial barriers, lack of continuity of care and poor therapeutic relationships.
CONCLUSIONS
The challenges in diabetes management in primary care have led to novel approaches, such as the development of Piki Te Ora. This model appears to be highly successful, with self-reports of differences in T2D disease management and symptomology after the programme. This model goes a long way to improving health outcomes, breaking down barriers and improving health outcomes for T2D patients and their whānau. It demonstrates a promising model for further implementation in primary care settings.
INVITED LONG ABSTRACT: Cancer incidence among those with diabetes in Aotearoa New Zealand: current and projected trends
Jason Gurney,1 Andrea Teng,1 James Stanley,1 Jeremy Krebs,2 Ross Lawrenson,3 Chunhuan Lao,3 on behalf of the Cancer and Chronic Conditions (C3) Research Group
1Department of Public Health, University of Otago, Wellington
2Department of Medicine, University of Otago, Wellington
3Te Huataki Waiora School of Health, University of Waikato, Hamilton
INTRODUCTION
Cancer and diabetes are increasingly prevalent, and it is not unusual for an individual to have both at the same time, given both are common and that one can increase the risk of the other. The occurrence of cancer among those with diabetes has significant ramifications to the person, the clinical team providing their care and the broader health system.
METHODS
For the period 2006–2019, we used national-level diabetes (Virtual Diabetes Register) and cancer (New Zealand Cancer Registry) data on nearly 5 million individuals over 44 million person-years of follow-up. We used cancer incidence among those with and without prevalent diabetes to project cancer incidence across the 2020–2044 period, using age-period-cohort modelling to account for factors driving trends in cancer incidence.
RESULTS
Cancer rates were highest among those with diabetes for 21 of the 24 most common cancers. The greatest differences in cancer incidence by diabetes status were in uterine, liver, pancreatic and kidney cancers, which all have a strong relationship with obesity. In terms of projected burden, cancers in people with diabetes were projected to more than double from 20,243 to 48,773, a 141% increase from 2015–2019 to 2040–2044. Age-standardised cancer incidence was projected to increase 2.4 times faster for people with diabetes (annual relative increase of 0.4% vs 0.2% for those without diabetes).
CONCLUSIONS
Our findings reinforce the fact that diabetes prevention activities are also cancer prevention activities and must therefore be prioritised and resourced in tandem.
“We are so happy because we have someone that will listen to us”: a qualitative evaluation of nurse practitioner led marae-based clinics
Keimarire Tibble-Brown (Ngāti Ranginui, Ngāti Pūkenga ki Manaia, Ngāti Porou, Ngāti Tūwharetoa),¹ Rebekah Crosswell (Whakatōhea),¹ Hine Loughlin (Ngāti Tūwharetoa),³ Hilde Mullins (Kahungunu ki Wairarapa),² Donna Foxall (Tainui),² Lynne Chepulis¹
¹Waikato Medical Research Centre, Te Huataki Waiora School of Health, University of Waikato, Hamilton
²Department of Nursing, Te Huataki Waiora School of Health, University of Waikato, Hamilton
³Whiria Te Tāngata, Tūrangi Te Huinga, Hirangi Marae, Taupō Te Rangiita Marae
INTRODUCTION
Due to colonisation and ongoing systemic impacts, Māori are three times as likely to develop type 2 diabetes (T2D) compared to non-Māori. Many individuals with T2D receive suboptimal disease management with Westernised biomedical models in primary care, leading to high rates of morbidity and mortality. Initiatives to address these inequities are urgently required. This research evaluates Māori T2D patients’ experiences of marae-based healthcare delivery.
METHOD
Kaupapa Māori informed semi-structured interviews were completed in December 2023, involving 11 Māori participants (nine male, two female) who were accessing healthcare at Whiria Te Tāngata, nurse practitioner led clinics in Taupō and Tūrangi. Interviews were audio recorded, transcribed orthographically and thematically analysed.
RESULTS
Unlike mainstream healthcare delivery, Whiria Te Tāngata healthcare delivery is grounded in Te Ao Māori and incorporates six overarching themes: whanaungatanga (relationship building), manaakitanga (support/care), aki (encouragement), mahi tahi (collaboration), whānau ora (whānau & community health) and tino rangatiratanga (self-determination). The removal of financial and transport barriers, lack of structured appointment times and involvement of whakapapa connections were described as the catalysts to the success. Participants reported contentment at the clinic, driven by holistic and patient-centred care. Further, they identified the importance of initiatives including health education in kura, kai sovereignty and investment in additional Māori health professionals.
CONCLUSIONS
While New Zealand’s mainstream model of healthcare delivery is failing many Māori with T2D, initiatives such as Māori-centric, marae-based health clinics may provide a promising model of care adjunct to primary care clinics to reduce health disparities and improve health outcomes for Māori with T2D.
Enhancing diabetes clinic attendance for high-risk patients in community-based settings
Amy Y Liu,1,2 Sam Sempers,2 Ole Schmiedel,1 Mele Kaufusi,1 Gina Berghan1
1Auckland Diabetes Centre, Te Whatu Ora Te Toka Tumai, Auckland, New Zealand
2Performance Improvement Team, Te Whatu Ora Te Toka Tumai, Auckland, New Zealand
INTRODUCTION
The global diabetes pandemic has profoundly impacted New Zealand. The Virtual Diabetes Register’s 2021 report reveals nearly 300,000 New Zealanders have diabetes, with projections of a 70–90% increase by 2040 and an annual healthcare cost of $3.5 billion. Māori and Pacific communities suffer disproportionately, experiencing 3–5 times higher rates of type 2 diabetes, compounded by socio-economic challenges. Notably, missed clinic appointments are as high as 43% in these groups, highlighting the need for improved clinic attendance in community settings.
METHOD
Using Lean Six Sigma methodology, our project involved diabetes staff and patients (both attending and missing appointments) from clinics with over 50% Māori and Pacific populations. We engaged in staff meetings, patient interviews and telephonic consultations. Solutions were generated and categorised using the PICK matrix into feasible, implementable, challenging and non-viable options.
RESULTS
Key findings showed varied communication preferences, indicating a need for consistent, frequent reminders. Flexibility was crucial, with clinicians encouraged to offer telehealth or rescheduling to manage personal disruptions. Participants desired more accessible appointments, suggesting extended clinic hours or days and the use of telehealth or joint clinics to reduce repeat visits. Empathy was also essential, with a focus on understanding and accepting last-minute cancellations to avoid stigmatising patients.
CONCLUSION
The study identifies effective strategies to improve diabetes clinic attendance in high-risk communities. These include enhanced communication, flexible scheduling, expanded telehealth options and compassionate handling of cancellations. These measures aim to improve healthcare outcomes, particularly for the Māori and Pacific populations heavily affected by the diabetes pandemic.
The “forgotten groups”: characterising type 2 diabetes in ethnic minority groups in Aotearoa New Zealand
Sara Mustafa,1 Mark Rodrigues,1 Ryan Paul,1,2 Rawiri Keenan,1 Rinki Murphy,3 Lynne Chepulis1
1Medical Research Centre, Te Huataki Waiora School of Health, University of Waikato, Hamilton
2Health New Zealand – Te Whatu Ora, Hamilton
3Faculty of Medical and Health Sciences, The University of Auckland; Te Whatu Ora Counties Manukau /Te Toka Tumai Auckland, New Zealand
BACKGROUND
Health data are often reported on in Aotearoa New Zealand using level 1 ethnicity data, such that any differences between minority ethnic groups are not reported. This study explores the characteristics and medication use of different Middle Eastern, Latin American and African (MELAA) and Asian ethnic groups with type 2 diabetes (T2D).
METHODS
Primary care data were collected by level 3 ethnicity for Waikato and Auckland patients aged 18–75 years with T2D (February 2021 to July 2022, 302 practices, n=57,743). Clinically indicated prescribing was defined as SGLT2i/GLP1RA and statins in renal and/or cardiovascular disease or equivalent risk, ACEi/ARB in renal disease and metformin in all with T2D.
RESULTS
A total of 9,143 Asian and 920 MELAA individuals were identified. For MELAA patients, clinically indicated prescribing for SGLT2i/GLP1RA (approximately 27%), metformin (approximately 80%), ACEi/ARBs (approximately 84%) and statins (86.2%) was comparable across ethnic groups (P>0.05) with no difference in mean HbA1c (58.4±14.6 mmol/mol). In Asian ethnicities, indicated SGLT2i/GLP1RA prescribing was lowest in Korean (7.7%) and highest in Fijian Indian (34%); (mean Asian 28.8%; P<0.001) and metformin prescribing ranged from 79.4–95.6%. Percent at HbA1c target (≤53mmol/mol) was lowest in Fijian Indian (29%) and highest in Chinese (55%; P<0.01).
CONCLUSIONS
Glycaemic control to target and clinically indicated prescribing differs in ethnic minorities with T2D in New Zealand. Care is needed to ensure that these groups are equally represented in health statistics so that culturally appropriate strategies can be designed to optimise care.
Success of the inaugural national NZSSD/University of Waikato Advanced Diabetes Management Course
Solita Donnelly,1 Bryan Gibbison,1 Claire Lever1,2 (Ngāi Tahu), Rachael Sampson,1 Ryan Paul1,2 (Ngāti Maru Hauraki)
1Aotearoa Diabetes Collective, Waikato, New Zealand
2Te Huataki Waiora, School of Health, University of Waikato, Hamilton, New Zealand
INTRODUCTION
The first national NZSSD/University of Waikato (UoW) Advanced Diabetes Management Course (ADMC) was delivered online by the Aotearoa Diabetes Collective between August–December 2023 to health professionals throughout Aotearoa. The ADMC consisted of 8 weekly 30–40-minute webinars and ≥8 weekly 30–40-minute case discussion sessions followed by a multiple-choice assessment.
METHODS
An online survey was sent in January 2024 to all participants in the 2023 ADMC (n=585 participants). Questions captured demographic data and 5-point Likert scale (1=poor/not at all, 5=excellent/extremely) ratings on perceptions of the course.
RESULTS
Approximately 56% of participants (n=325) completed the survey, with 15% being general practitioners, 7% nurse practitioners, 44% registered nurses, 17% pharmacists, 9% dietitians and 8% other professions, with responses from all old district health board regions. Feedback was overwhelmingly positive with mean scores all ≥4.6/5 for overall quality of the ADMC, organisation, content and delivery of the ADMC, focussing on improving health outcomes for Māori and Pacific, improvements in own clinical practice and likelihood of recommending course to peers. Approximately 35% reported difficulty accessing the UoW online platform at some point and 83% were keen for points towards a postgraduate qualification. Only 59% (n=585) of those who registered for the ADMC attended at least one session, but >80% (n=477) of these participants completed all components.
CONCLUSIONS
The inaugural national NZSSD/UoW ADMC was well received and led to a subjective improvement in clinical practice. Improvements to the online platform, academic accreditation and optimising registration are underway for the 2024 ADMC.
Specialist nursing care and real-time continuous glucose monitoring in reducing cardiovascular risk in high-risk adults with insulin-requiring type 2 diabetes: a sub-analysis of the 2GO-CGM study
Henry Eglinton6 (Ngāpuhi), Claire Lever1,2,3 (Ngāi Tahu), Jonathan Williman,4 Alisa Boucsein,5 Antony Watson,6 Rachael Sampson,2,3 Oscar Sergel-Stringer,5 Celeste Keesing,2 Benjamin Wheeler,5,7 Martin de Bock,6,8 Ryan Paul1,2,3 (Ngāti Maru)
1Te Huataki Waiora, School of Health, University of Waikato, Hamilton, New Zealand
2Waikato Regional Diabetes Service, Te Whatu Ora Waikato, Hamilton, New Zealand
3Aotearoa Diabetes Collective, Waikato, New Zealand
4Biostatistics and Computation Biology Unit, University of Otago, Christchurch, New Zealand
5Department of Women’s and Children’s Health, University of Otago, Dunedin, New Zealand
6Department of Paediatrics, University of Otago, Christchurch, New Zealand
7Department of Paediatrics, Te Whatu Ora Southern, Dunedin, New Zealand
8Department of Paediatrics, Te Whatu Ora Waitaha Canterbury, Christchurch, New Zealand
INTRODUCTION
We assessed the effects of a diabetes specialist nurse led model of care and real-time continuous glucose monitoring (rtCGM) on predicted cardiovascular disease (CVD) risk in type 2 diabetes (T2D) in a subanalysis of the 2GO-CGM study.
METHODS
The 2GO-CGM study randomised 70 people with insulin-requiring T2D with suboptimal glycaemic control to rtCGM or routine care with self-monitoring of blood glucose levels (SMBG) for 12 weeks. Both groups had their glucose-lowering and cardiovascular therapies optimised by prescribing-capable diabetes specialist nurses. An extension phase is ongoing with all participants using rtCGM. Predicted CVD risk was calculated at baseline and RCT end using the NZSSD CVD/ESRD calculator. Actual event rate was compared to baseline predicted event rate during the extension phase.
RESULTS
Predicted CVD scores were compared in all participants with complete data (n=55), who were predominantly Māori (54.5%). CVD risk scores improved across both groups (absolute risk reduction rtCGM 2.196±1.471%, p=0.005 and SMBG 1.376±0.861%, p=0.003), with no between-group difference (p=0.24). Improvements in CVD risk correlated significantly with increased HDLc and reduced HbA1c and microalbuminuria (p<0.05 versus baseline). Mean follow-up at time of analyses was 1.6±0.1 years, with an actual event rate of 0.63/year compared to the predicted 1.6 events/year prior to rtCGM initiation.
CONCLUSIONS
A specialist nurse supported care model, including rtCGM application, can reduce cardiovascular risk in a high-risk population with insulin-requiring T2D.
DECLARATIONS
Study funded by Dexcom.
M de Bock: received honoraria, advisory board member for Dexcom.
R Paul: advisory board member for Dexcom.
Extended use of real-time continuous glucose monitoring in adults with insulin-requiring type 2 diabetes: the 12-week continuation phase following the 2GO-CGM randomised controlled trial
Claire Lever1,2,3 (Ngāi Tahu), Jonathan Williman,4 Alisa Boucsein,5 Antony Watson,6 Rachael Sampson,2,3 Pip Milford-Hughes,5 Celeste Keesing,2,8 Benjamin J Wheeler,5,7 Martin de Bock,6,9 Ryan Paul1,2,3 (Ngāti Maru, Hauraki)
1Te Huataki Waiora, School of Health, University of Waikato, Hamilton
2Waikato Regional Diabetes Service, Health New Zealand – Te Whatu Ora Waikato
3Aotearoa Diabetes Collective, Waikato
4Department of Population Health, University of Otago, Christchurch
5Department of Women’s and Children’s Health, Dunedin School of Medicine, University of Otago, Dunedin
6Department of Paediatrics, University of Otago, Christchurch
7Department of Paediatrics, Te Whatu Ora Southern, Dunedin
8Pinnacle Midlands Health Network, New Zealand
9Department of Paediatrics, Health New Zealand – Te Whatu Ora Waitaha Canterbury
INTRODUCTION
The impact of real-time continuous glucose monitoring (rtCGM) on glycaemia for Māori and non-Māori with type 2 diabetes in Aotearoa is unestablished. The 2GO-CGM study assessed efficacy and safety of rtCGM in a cohort of adults with insulin-requiring type 2 diabetes.
METHODS
Both groups of a 12-week randomised controlled trial comparing rtCGM (Dexcom G6) with self-monitoring of blood glucose (SMBG) entered a 12-week continuation phase where SMBG users (designated the SMBG-rtCGM group) crossed over to use rtCGM alongside rtCGM users (the rtCGM-rtCGM group). Analyses of all 24 weeks of data, including within-subject and between-group differences, were conducted to examine an overall treatment effect of rtCGM versus SMBG.
RESULTS
Sixty-one participants completed the 24-week study period (52% Māori, 57% female, median age 54 (range 16–69) years. Baseline-adjusted mean TIR was 15.2% (95% CI 10.4–20.1; p=<0.001) higher in the rtCGM users versus SMBG users. Mean HbA1c (±SD) decreased in both groups from 85 (19) mmol/mol to 59 (11) mmol/mol in the rtCGM arm and from 82 (12) mmol/mol to 59 (12) mmol/mol in the SMBG arm (p<0.001 for both). One participant withdrew in the continuation phase due to unmanageable skin reactions to CGM device. There were no severe hypoglycaemia or ketoacidosis events in either group.
CONCLUSIONS
Use of rtCGM over 24 weeks demonstrates safe and sustained glycaemic improvement in Māori and non-Māori rtCGM users.
SGLT2I/GLP1RA agents appear to be improving clinical outcomes in New Zealand patients with type 2 diabetes and cardiovascular/renal disease
Lynne Chepulis,1 Rawiri Keenan,1 Mark Rodrigues,1 Leanne Te Karu,2 Penny Clark,3 Rinki Murphy,2,4 Tim Kenealy,2 Jo Scott-Jones,5 Allan Moffit,6 Ross Lawrenson,1,7 Ryan Paul1,7
1Medical Research Centre, School of Health, University of Waikato, Hamilton, New Zealand
2Faculty of Medical and Health Sciences, The University of Auckland, New Zealand
3Northcare Medical Centre, Hamilton, New Zealand
4Health New Zealand Counties Manukau /Te Toka Tumai Auckland, New Zealand
5 Midlands Health Network, Hamilton, New Zealand
6 ProCare Health Limited, Auckland, New Zealand
7 Health New Zealand Waikato, Hamilton, New Zealand
BACKGROUND
Type 2 diabetes (T2D) associates with significant cardiovascular/renal disease (CVRD) risk and patients must be optimally managed to optimise health outcomes. This study aimed to evaluate the impact of newly funded access to GLP1RA/SGLT2i on BP, LDL-C and HbA1c in patients with T2D and CVRD.
METHODS
Waikato/Auckland primary care data were collected for those 18–75 years with T2D during 2021–2022 (302 general practice clinics). We reviewed mean values and percent of patients at target (%PAT) for BP (≤130/80 mm/Hg), LDL-c (≤1.8 mol/L) and HbA1c (≤53 mmol/mol; 7%) at July 2022 vs January 2021 in those with CVRD who did/did not initiate SGLT2i/GLP1RA therapy (≥2 prescriptions).
RESULTS
Overall, 8,036 of 17,068 CVRD patients (47.1%) initiated SGLT2i/GLP1RA therapy, with higher uptake in NZ Māori compared to NZ European patients (54.5% vs 41.8%; P<0.001). In patients with CVRD who initiated therapy, the %PAT increased for HbA1c (10.7% to 15.8% [+5.1%]), LDL-c (43.5% to 44.6% [+1.1%]) and BP (39.7% to 41.5% [+1.8%]) (all P<0.05) compared to minimal improvements of 0.1–0.3% in patients with CVRD who did not commence therapy. Mean HbA1c decreased by 4.0 vs 0.3mmol/mol and LDL-c by 0.1 vs 0.0mmol/L in those prescribed vs not prescribed SGLT2i/GLP1RA (both P<0.05) though no change was observed in BP.
CONCLUSION
SGLT2i/GLP1RA use appears to be associated with improved glycaemic and cardiovascular markers in patients with T2D and CVRD. Further research is required to evaluate the longer-term impact of these medications on clinical outcomes and hospitalisation rates.
Glucose and psychosocial outcomes 12 months following transition from multiple daily injections to advanced hybrid closed loop in youth with type 1 diabetes and suboptimal glycaemia
Venus Michaels,1* Alisa Boucsein,1* Antony Watson,2 Carla Frewen,1 Olivia Sanders,2 Jillian Haszard,3 Shirley Jones,1 Philippa Milford-Hughes,1 Martin de Bock,2,4 Benjamin Wheeler1,5
1Department of Women’s and Children’s Health, University of Otago, Dunedin, New Zealand
2Department of Paediatrics, University of Otago, Christchurch, New Zealand
3Biostatistics Centre, University of Otago, Dunedin, New Zealand
4Health New Zealand – Te Whatu Ora, Christchurch, New Zealand
5Health New Zealand – Te Whatu Ora, Dunedin, New Zealand
*Co-first author
OBJECTIVES
To investigate 12-month glycaemic and psychosocial changes following transition from multiple daily injections (MDI) to advanced hybrid closed-loop (AHCL) therapy in youth (aged 13–25 years) with type 1 diabetes and suboptimal glycaemia (glycated haemoglobin [HbA1c] ≥8.5% [69 mmol/mol]).
METHODS
Prospective, single-arm, dual-centre study in 20 participants. Extension phase outcomes reported after 12 months, including HbA1c, time in glycaemic ranges, AHCL system performance and psychosocial questionnaires assessing quality of life, diabetes treatment and sleep.
RESULTS
After 12 months, 19 out of 20 participants continued to use AHCL. Average time-in-range 70–180mg/dL (3.9–10.0mmol/L) improved from 27.6%±13.2% to 62.5%±11.4%. This translated to an average 2.5 percentage-point (27.1mmol/mol) improvement in HbA1c from 10.5%±2.1% (91.2mmol/mol) at baseline to 8.0%±0.9% (64.1mmol/mol) at 12 months. Psychosocial questionnaires and very high HbA1c at study entry indicated significant diabetes-associated burden for both individuals and parents. Safety data were reassuring with a diabetic ketoacidosis rate of 0.15 per participant-year after 12 months of AHCL (compared to 0.25 per participant-year in the 12 months before the study).
CONCLUSIONS
After 12 months of AHCL usage, this study highlights the potential for substantial and sustained glycaemic and psychosocial improvements among individuals experiencing considerable diabetes burden and suboptimal glycaemia following their switch from MDI to AHCL.
Relationship between carbohydrate counting and carbohydrate announcement to glycaemic control in young people using AHCL insulin delivery
Madeleine Gray,1 Alisa Boucsein,2 Yongwen Zhou,2,3 Jillian J Haszard,4 Craig A Jefferies,5,6 Esko J Wiltshire,7,8 Sara E Styles,9 Hamish R Crocket,10 Maheen Pasha,11 Goran Petrovski,11 Ryan G Paul,10,12 Martin I de Bock,13,14 Benjamin J Wheeler2,15
1Student at Dunedin School of Medicine, University of Otago, Dunedin, New Zealand
2Department of Women’s and Children’s Health, University of Otago, Dunedin, New Zealand
3Department of Endocrinology, Institute of Endocrine and Metabolic Diseases, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, Clinical Research Hospital of Chinese Academy of Sciences (Hefei), University of Science and Technology of China (USTC), Hefei, Anhui, 230001, China
4Biostatistics Centre, University of Otago, Dunedin, New Zealand
5Starship Child Health, Te Whatu Ora Te Toka Tumai Auckland, Auckland, New Zealand
6Liggins Institute and Department of Paediatrics, The University of Auckland, Auckland, New Zealand
7Department of Paediatrics and Child Health, University of Otago Wellington, Wellington, New Zealand
8Te Whatu Ora Capital, Coast and Hutt Valley, Wellington, New Zealand
9Department of Human Nutrition, University of Otago, Dunedin, New Zealand
10Te Huataki Waiora School of Health, University of Waikato, Hamilton, New Zealand
11Sidra Medicine, Doha, Qatar
12Waikato Regional Diabetes Service, Te Whatu Ora Waikato, Hamilton, New Zealand
13Department of Paediatrics, University of Otago, Christchurch, New Zealand
14Te Whatu Ora Waitaha Canterbury, Christchurch, New Zealand
15Te Whatu Ora Southern, Dunedin, New Zealand
INTRODUCTION
Little has been investigated regarding the predictors of glycaemic control for individuals with high-risk glycaemia after transitioning to the Minimed 780G AHCL system. This project investigates the relationship between glucose control and food announcement behaviour and method in youth (7–25) with type 1 diabetes and elevated glycaemia.
METHODS
This project takes data from two studies (n=100, n=64 in this abstract), Co-Pilot and AHCL in high-risk youth, which both targeted youth with high-risk glycaemia (HbA1c ≥8.5% [69 mmol/mol]) and had similar inclusion/exclusion criteria. Measures of glycaemic control (HbA1c, time in range [%CGM 3.9–10mol/L]), meals and carbohydrates input per day and time in automation were gathered over a 3-month period post-transition to AHCL.
RESULTS
On average, HbA1c decreased by -29.0±22.6 mmol/mol. Meals inputted per day predicted glycaemic control, with the greatest change in HbA1c seen in those entering 3 or more meals/day (-34.2±21.1mmol/mol). Those entering <1 meal per day still saw HbA1c improvement (-22.8±49.6mmol/mol). Total carbohydrate entered per day was also associated with decrease in HbA1c, though with a more complex relationship. Participants spending more than 80% of time automation also saw greatest HbA1c improvements.
CONCLUSIONS
Participants in these studies on average saw a significant decrease in HbA1c after transitioning to AHCL, with even those inputting minimal meals seeing on average a >20mmol/mol improvement in HbA1c. However, predictors for optimal improvement remain frequent meal announcements and high use of automation.
The Child Disability Allowance is used to subsidise continuous glucose monitoring in type one diabetes
Sara Mustafa,1 Lynne Chepulis,1 Rawiri Keenan1 (Te Atiawa, Taranaki) Rebekah Crosswell1 (Whakatōhea, Ngati Patumoana), Ryan Paul1,2 (Ngati Maru), Hamish Crocket1
1Te Huataki Waiora School of Health,
University of Waikato, Hamilton, New Zealand
2Waikato Regional Diabetes Service, Te Whatu Ora Waikato, Hamilton, New
Zealand
INTRODUCTION
The child disability allowance (CDA) is a non-means tested benefit that all whānau with a child aged <18 years with type one diabetes (T1D) are eligible to receive. However, it is not known how many whānau access the CDA, nor is it known what the CDA is used for in relation to T1D.
METHODS
A 40-item survey was developed to gather demographic information along with information about access to, and use of, the CDA in relation to T1D. We report on current survey completions from recruitment via New Zealand T1D Facebook groups.
RESULTS
Ninety parents completed the survey. Most children were European (81.6%), with 6.9% Māori and 5.7% Pacific. Mean duration of diabetes was 2.4 years. Sixty point four percent of children used an insulin pump and 86.8% used a CGM. Losing access to the CDA would impact CGM use severely for 71.0% and moderately for 15.9% of whānau and impact quality of food purchased severely for 39.1% and moderately for 21.7% of whānau.
CONCLUSION
In this sample of families, the CDA is a key source of funding for CGM. Further recruitment is planned via Diabetes New Zealand and regional diabetes youth organisations. A larger sample will facilitate an equity analysis. Further research should examine the impacts of “ageing out” from the CDA at 18 years on access to CGM for young adults with T1D.
Insulin pump initiation in a naïve population
Rosemary M Hall, Michell Krawczyk
Diabetes service, Tui Te Ora, Te Whatu Ora Tairāwhiti, New Zealand
INTRODUCTION
A multidisciplinary specialist diabetes service, integrated into primary care, has recently been established in Te Whatu Ora Tairāwhiti. In 2021 a review described it as a “service in crisis.” There were 41 adults with T1DM with a mean (SD) HbA1c 79.4 (25.2) mmol/mol; five were using an insulin pump. The diabetes team and patients were not familiar with availability of insulin pumps, or confident with initiation or management. We sought to change this, identifying opportunities for education, mentoring and telehealth to develop an insulin pump service.
METHODS
This retrospective audit aimed to identify all adult insulin pump users in the Tairāwhiti diabetes service, to describe the population initiated on a pump, use of CGM and hybrid closed loop, and changes in HbA1c during this time.
RESULTS
Tairāwhiti currently has 98 adults with T1DM managed within the specialist diabetes service. Nineteen (18.4%) use an insulin pump.
Current pump users are: 13 female, six male; mean age 44 years (range 23–76); five Māori, 14 Pākehā. Fourteen use a CGM and 10 use a hybrid closed loop system.
Mean (SD) HbA1c prior to pump initiation was 69.5 (16.6) mmol/mol. At 3 months HbA1c was 57.2 (11.6) and the most recent HbA1c was 58.1 (10.4).
There is an increasing number of people waiting for a pump, limited by staff resources.
CONCLUSIONS
Proactive development of an insulin pump service in a remote population is possible with the use of local and remote specialist support, and active education. For patients, developing a trusting relationship is key to successful initiation and management.
