ARTICLE
Vol. 133 No. 1509 |
Does screening for myopia in New Zealand meet screening programme criteria?
Myopia is the most common ocular problem internationally and prevalence is increasing.
Full article available to subscribers
Myopia is the most common ocular problem internationally and prevalence is increasing. Research suggests myopia currently affects 23% of the world population, with estimates of 49% affected by 2050.1 In certain East Asian countries myopia affects 90% of young adults.2 Nearly a third (30%) of 17-year-olds in Sydney are myopic, which represents a doubling of prevalence from a decade earlier.3 The only published New Zealand data come from a survey (1984) with a prevalence of myopia of 4.2% in Dunedin 11-year-olds.4 Unpublished data from the same cohort at age 45 shows prevalence of myopia of 34.1%.5 The increasing prevalence of myopia is linked primarily to environmental factors including near work activities and decreased outdoor time.6 High myopia increases the risk of irreversible vision loss through predisposition to ocular changes, including cataract, glaucoma, retinal detachment and myopic macular degeneration.1 Even a low myope (one to three dioptres) is twice as likely to develop myopic maculopathy, glaucoma or posterior subcapsular cataract, and at least three times as likely to develop retinal detachment.7–9
Petty et al suggested that the risks associated with myopia in New Zealand are under-appreciated by the medical, educational and public health community.10 Current treatment is aimed at correcting refractive error rather than preventing axial length elongation. Attempting to prevent myopia progression offers an opportunity to decrease the burden of myopia on individuals and wider society.10 Current New Zealand national vision screening guidelines published in 2014 state two purposes: to identify children with amblyopia at an age when treatment might be effective; and to identify and refer children with reduced visual acuity for further assessment. Screening consists of a ‘B4 School Check’(<age 4) and Year 7 (age 11) vision screening. Visual acuity testing is measured and referrals are made to optometrists or ophthalmologists if screening requirements are not met.11 The 2010 Eye Health Workforce Service Review suggested improvements are needed in vision screening. Health Workforce New Zealand supports the rationalisation and standardisation of child vision screening services in New Zealand.12
The aim of a screening programme is to identify disease in a community early, to enable earlier intervention to avoid suffering from the disease.13 Proposed screening programmes must be carefully evaluated to avoid potential adverse effects of screening.14 The aim of this paper is to evaluate the validity of screening for childhood myopia in New Zealand utilising the Wilson and Jungner criteria. The Wilson and Jungner criteria published in 1968 is a method for considering the utility of screening programmes for disease control.15 Although newer policy tools are available, the validity of the criteria remains undisputed today.13 Ideally all 10 of the Wilson and Jungner criteria should be met before a screening programme is adopted. If there is uncertainty or failure to meet criteria, then further research or pilot screening programmes should be conducted. The criteria have different weights in different settings; for example, in a wealthier jurisdiction there may be less emphasis on cost-effectiveness. Furthermore, issues such as “service availability” will be more important in rural settings compared with highly urbanised settings.13 Below, the criteria are used to examine the validity of screening for childhood myopia in New Zealand.
The condition sought should be an important health problem
Myopia is the most common cause of distance vision impairment internationally and prevalence is increasing.1 Individuals not treated endure lifelong visual impairment and increased risk of blindness.7–9 Financial cost to individuals and society are significant.16,17 Refractive error and low vision are ranked number five on the World Health Organization priority eye disease list.18 Myopia ranks as the third most common long-term health condition in Australian children.19
There should be an accepted treatment for patients with recognised disease
Researched methods to reduce the rate of myopia progression include behavioural, pharmacological and optical approaches.20 The International Myopia Institute concluded that modalities within all three approaches are worthy of further exploration, and variability in treatment efficacy exists at an individual level.21 Increased near work and lack of outdoor activity are risk factors for myopia progression, and therefore are the targets of behavioural intervention.6 A 2017 meta-analysis showed increased outdoor time reduced myopia onset and subsequent progression.22
Pharmacologically, multiple antimuscarinic drugs have been studied. Low-dose atropine has proven most promising with clinical efficacy, and tolerability with minimal adverse effects.23–25 Chia et al concluded that low-dose atropine (0.01%) for periods up to five years is a clinically viable treatment.26 Their results showed mean myopia progression at five years (1.38 D) in children receiving atropine 0.01% was similar to placebo eyes at 2.5 years (1.40 D), suggesting a 50% reduction in progression of spherical equivalence.26 However, it is important to note that the effect of low-dose atropine (0.01%) on slowing axial elongation has not been convincingly established.27 Issues also exist around possible myopic rebound with treatment cessation, and requirement for long-term adherence.23–25 The recent one-year results of the LAMP study conclude that 0.05%, 0.025% and 0.01% atropine eye drops were well tolerated, and reduced myopia progression with a concentration-dependent response.28 0.05% atropine was the most effective in controlling spherical equivalence progression and axial length elongation over a period of one year.28 Results showed a larger axial length change at one year in the placebo group (0.41 +/- 0.22mm) than in the 0.05% (0.20+/-0.25mm), 0.025% (0.29+/-0.20mm) and 0.01% (0.36+/-0.29mm)atropine groups (P<0.001). Pairwise comparison of axial length change between the 0.01% atropine and placebo groups was not statistically significant(P<0.18).28
Various optical treatments have been investigated for myopia treatment. The majority have shown some efficacy in small studies, although some systematic reviews question viability. The International Myopia Institute suggests that orthokeratology lenses slow myopia by approximately 30–60%.21 A 2015 systematic review also suggested orthokeratology is viable for myopia treatment.29 A further meta-analysis in 2018 concluded that adoption of orthokeratology for myopia control in children requires careful thought, given the risk-benefit ratio combined with the low compliance of the patients has not yet delivered unidirectional results.25 Benefits of orthokeratology include not having to wear a vision correction during the day.21 Issues include risk-benefit ratio with increased risk of keratitis, possible myopic rebound on cessation, and compliance.24 The International Myopia Institute suggested multifocal soft contact lenses are expected to slow myopia progression by about 30–50%.21
Available guidelines from the International Myopia institute and the Brien Holden Institute advise clinicians on implementing methods of intervention for myopia control using available evidence.30,31 Given existing uncertainties around optical and pharmacological treatment, further randomised clinical trials which clearly define appropriate myopia treatment modality and timing will be integral in ensuring clinical guidelines are robust. New Zealand Myopia Action Group (NZMAG) is a panel of experts with an aim to reduce the impact of myopia in New Zealand. They aim to create New Zealand-specific guidelines adapted from the aforementioned international guidelines.
Facilities for diagnosis and treatment should be available
Vision screening programmes already exist through New Zealand Vision Hearing Technicians, ie, the B4 School check(age <4) and year 7 (age 11) vision screening.12 The B4 School Check is performed in conjunction with hearing testing. Once an individual is diagnosed with myopia, they would be referred to publicly funded optometry or ophthalmology clinics for ongoing management. The New Zealand Myopia Action Group (NZMAG) is advocating for Pharmac to fund low-dose atropine. Current monthly cost of low-dose atropine (0.01%) in New Zealand is approximately $50/month per individual.32
There should be a recognisable latent or early symptomatic stage
Myopia can be easily identified at an early stage through photorefraction combined with an accepted definition of myopia.33–35
There should be a suitable test or examination
A variety of reliable and user friendly vision screening devices exist including PlusoptiX, Retinomax, WelchAllyn Spot Vision Screener, Topcon KR-8900, Nidek ARK-510A and Huvitz HRK-7000A. Photorefraction is advantageous over visual acuity given it obtains an estimation of severity of myopia.33 PlusoptiX photorefraction vision screening device aims to empower primary healthcare providers to detect prevalent vision disorders in children as early as possible. Screening with PlusoptiX is possible from the age of five months and meets the guidelines of the American Academy of Pediatrics.33 PlusoptiX A12 has been shown to yield a good estimation of the spherical and cylindrical component of refractive errors compared to cycloplegic examination, with greater accuracy in the myopic and astigmatic subgroups compared with hyperopic subgroups.36 The sensitivity, specificity, positive and negative predictive values for myopia were, respectively, 86%, 93%, 82% and 94%, with an average overestimation of myopia by 0.05 D.36
The test should be acceptable to the population
Photorefraction vision screening devices offer a reliable, fast, non-invasive, user friendly screening method that is acceptable to the population.33–36
The natural history of the condition,including development from latent to declared disease, should be adequately understood
Our understanding of most medical conditions is often in a state constant evolution. It could be argued that we have an adequate understanding of myopia. Myopia is variably defined as a refractive error equal to or worse than −0.25 to −1.00 D, and is often graded according to severity and age of onset.37 Severity of myopia is generally categorised as low (−0.50 to −2.99 D), moderate (−3.00 to −5.99 D) or severe (worse than or equal to −6.00).38
Myopia is understood as a multifactorial disease influenced by interplay between genetic and environmental factors.24 In 2016 approximately 70 genetic loci had been linked to primary myopias.39 Animal models have shown response of axial eye growth in order to compensate for imposed defocus.40 Various bio-molecular pathways have been investigated;for example, dopamine plays an important role in the development of experimental myopia.41 Myopia usually first occurs in school-age children. This is defined as youth onset myopia with onset prior to age 20. Because the eye continues to grow during childhood and adolescence,myopia typically progresses until about the age of 20 years.39
There should be an agreed policy on whom to treat as patients
A 2018 survey of paediatric ophthalmologists internationally concluded “there is no consensus of the best treatment method in order to prevent myopia progression, when to begin treatment, and in whom treatment should be tailored according to one’s genetic background”.20 In August 2018, the Brien Holden Vision Institute released “Guidelines for Myopia Management” (Figure 1). Described as an “evidence-based, free, easy-to-use, practical tool developed to assist the busy eye-care professional manage patients with myopia”. The guidelines inform practitioners of appropriate diagnostic tests, risk assessment, myopia management options and scheduling of follow-up visits and tests.30 In February 2019, the International Myopia Institute released a “Clinical Management Guidelines Report”. The report suggests effective guidelines for myopia control require understanding of the epidemiology of myopia, risk factors, interventions, as well as an appropriate communication strategy. The report detailed an evidence-based best practice approach to myopia control, including risk factor identification, examination, selection of treatment strategies and guidelines for ongoing management.31 They highlighted that there is currently no research investigating the appropriate point of intervention based on age or refractive status. They suggested that appropriate treatment should be selected based on patient specific factors, with multiple risk factors requiring more strategic management and closer monitoring. Their guidelines suggest reassessment every six months to monitor efficacy and safety, with more frequent visits within the first six months.41 New Zealand Myopia Action Group is a panel of experts with an aim to reduce the impact of myopia in New Zealand. They are refining New Zealand-specific guidelines adapted from aforementioned international guidelines.
Figure 1: Guidelines for Myopia Management, Brien Holden Institute.40
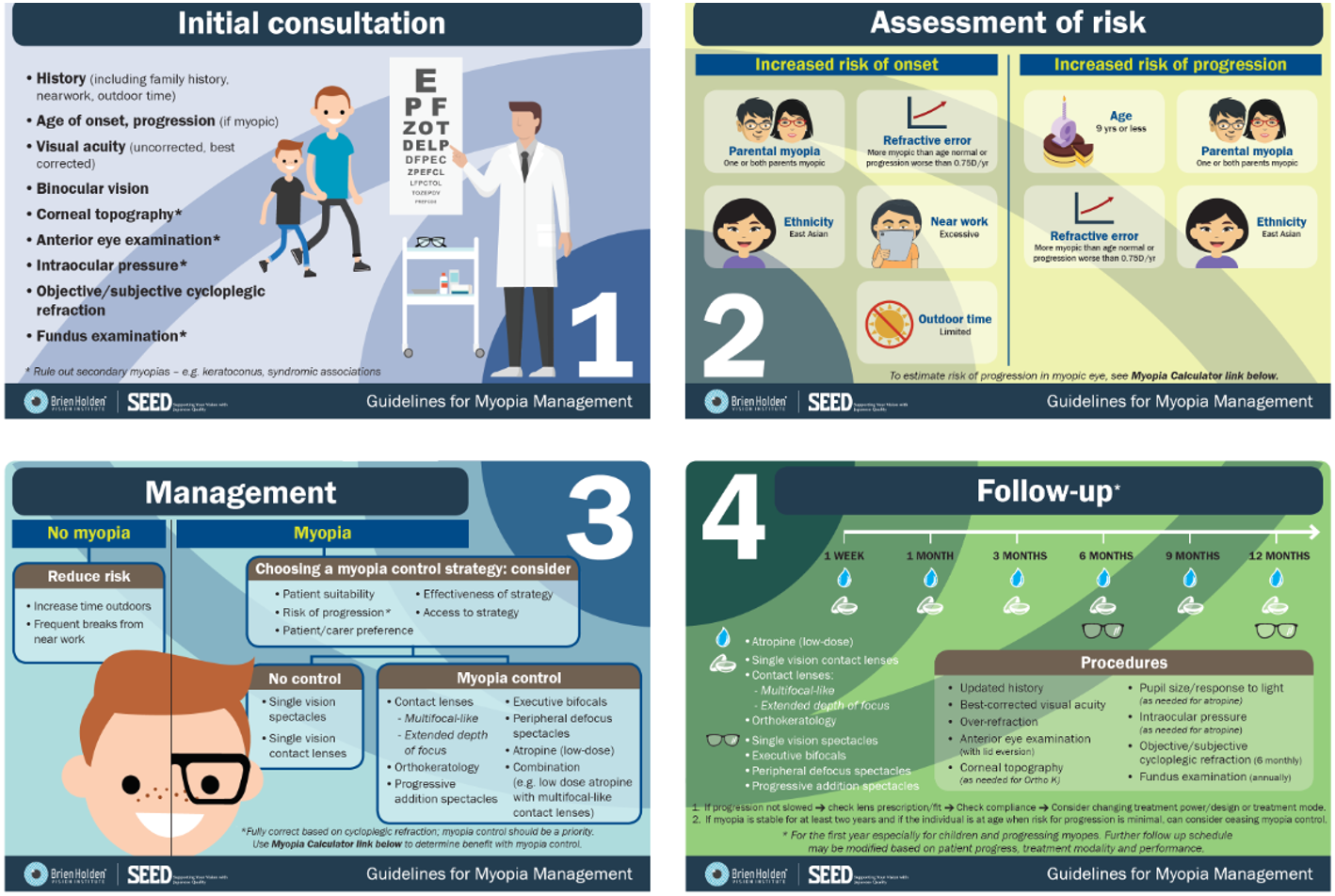
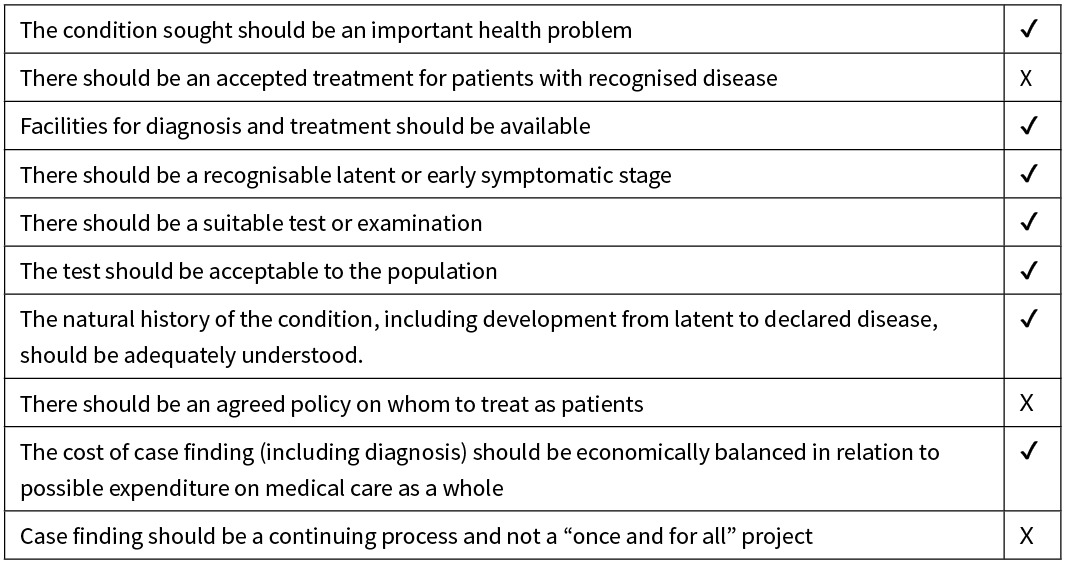
Table 1: Validity of Screening for Childhood Myopia in New Zealand—Wilson and Jungner Criteria.15
The cost of case finding (including diagnosis) should be economically balanced in relation to possible expenditure on medical care as a whole
Myopia imposes considerable economic burden on patients, public health systems and wider society. Analyses performed in Australia and the US have shown the cost of refractive correction is the highest among ocular diseases.42 Estimates suggests annual global loss of $202 billion of gross domestic product due to uncorrected refractive error.17 A study of Singaporean adults with myopia estimated a cost of US$709 per person per year. This equates to lifetime cost to an individual with disease for 80 years of US$17,020.43 Costs of an effective screening programme include staffing, administration, screening facilities and vision screening equipment. Facilities to provide ongoing monitoring of efficacy and safety would be required.41 Efficacy would be monitored by axial length measurement and refraction. Safety monitoring of atropine would require intraocular pressure testing and pupil function, and orthokeratology would require corneal topography.41 Treatment costs of identified cases with low-dose atropine are likely to be low.30 Nevertheless,there is still a need for real-world cost-effectiveness studies of using antimuscarinic drugs for slowing progression of myopia.
Case finding should be a continuing process and not a “once and for all” project
We propose adjusting the year 7 (age 11) vision screening program to include a one-off myopia check. We therefore accept failure of our proposal to meet this requirement.
Conclusion
There is a worldwide myopia epidemic which requires urgent attention to reduce vision impairment, blindness and costs to wider society.1 The risks associated with myopia are under-appreciated in New Zealand, and treatments need to be refocused from correcting refractive error to preventing axial length elongation.10 We’ve shown that under scrutiny of the Wilson and Jungner criteria, the concept of a screening programme for myopia in New Zealand performed relatively well, and so should be considered further. What is needed is further results from randomised clinical trials which clearly establish the appropriate myopia treatment modalities and timing. The New Zealand Myopia Action Group will then work to establish New Zealand specific myopia management guidelines. Following this, a trial should be conducted in the New Zealand setting to assess real-world feasibility and cost-effectiveness of a screening programme to identify early myopia and provide treatment to slow progression. Adjustments could be made to the already available year 7 (age 11) screening programme, consisting of suitable reduction of screening age, and introduction of autorefractors. This would also serve to help accurately document the prevalence of myopia in New Zealand. Addressing the myopia epidemic is a hot topic internationally, with a high volume of ongoing discussion and research. We need to act now, remain active in international discussion, and have an evidence-based approach which is adaptable to new findings.
Aim
The purpose of this paper is to assess whether screening for myopia in New Zealand is valid under scrutiny of the Wilson and Jungner criteria. There is a worldwide myopia epidemic which requires urgent attention to reduce vision impairment, blindness and costs to wider society. The risks associated with myopia are under-appreciated in New Zealand, and treatments need to be refocused from correcting refractive error to preventing axial length elongation.
Methods
The Wilson and Jungner criteria was used to assess the validity of screening for myopia in New Zealand through review of the latest evidence relevant to each point within the criteria.
Results
We found that the screening for myopia in New Zealand met 7 out of 10 of the Wilson and Jungner criteria.
Conclusion
The concept of a screening programme for myopia in New Zealand performed relatively well, and should be considered further. Further randomised clinical trials, which clearly identify the appropriate treatment modalities and timing, would allow the establishment of robust New Zealand specific myopia management guidelines. We would then suggest a trial of a screening programme in New Zealand setting to assess real-world feasibility and cost-effectiveness to identify early myopia and provide treatment to slow progression. Adjustments could be made to the already available screening programme, consisting of suitable reduction of screening age, and introduction of autorefractors.
Authors
Ben Wilkinson, Ophthalmology Registrar, Gisborne Hospital, Tairāwhiti District Health Board, Gisborne; Graham Wilson, Consultant General and Paediatric Ophthalmologist, Gisborne Hospital, Tairāwhiti District Health Board; Clinical Senior Lecturer, Faculty of Medical and Health Sciences, University of Otago; Principal Investigator, Vision, The Dunedin Study.Correspondence
Ben Wilkinson, Department of Ophthalmology, Gisborne Hospital, 421 Ormond Rd, Gisborne.Correspondence email
bwilkinson.md@gmail.comCompeting interests
Nil.1. Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016 May; 123(5):1036–42.
2. Pan C-W, Dirani M, Cheng C-Y, et al. The age-specific prevalence of myopia in Asia: a meta-analysis. Optom Vis Sci. 2015 Mar; 92(3):258–66.
3. French AN, Morgan IG, Burlutsky G, et al. Prevalence and 5- to 6-year incidence and progression of myopia and hyperopia in Australian schoolchildren. Ophthalmology. 2013 Jul; 120(7):1482–91.
4. Beauchamp G. Refractive error, IQ and reading ability: A longitudinal study from age seven to 11: by SM Williams, GF Sanderson, DL Share, and PA Silva. Dev Med Child Neurol 30: 735–742, 1988. Surv Ophthalmol. 1989; 34(3):234–5.
5. Wilson G. (2019). Dunedin multidisciplinary health and development study p45. Unpublished raw data.
6. Lin Z, Gao TY, Vasudevan B, et al. Near work, outdoor activity, and myopia in children in rural China: the Handan offspring myopia study. BMC Ophthalmol. 2017 Nov 17; 17(1):203.
7. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012 Nov; 31(6):622–60.
8. Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999 Oct; 106(10):2010–5.
9. Vongphanit J, Mitchell P, Wang JJ. Prevalence and progression of myopic retinopathy in an older population. Ophthalmology. 2002 Apr; 109(4):704–11.
10. Petty AD, Wilson G. Reducing the impact of the impending myopia epidemic in New Zealand. N Z Med J. 2018 Dec 14; 131(1487):80–5.
11. Ministry of Health. National Vision and Hearing Screening Protocols. MOH. New Zealand. Revised 2014. 34.
12. Health Workforce New Zealand. Eye Health Workforce Service Review. HWNZ. New Zealand: August 2010. 52.1.
13. Andermann A, Blancquaert I, Beauchamp S, Déry V. Revisiting Wilson and Jungner in the genomic age: a review of screening criteria over the past 40 years. Bull World Health Organ. 2008 Apr; 86(4):317–9.
14. O’Sullivan et al. Overtesting and undertesting in primary care: a systematic review and meta-analysis. BMJ Open. 2018 Feb 11; 8(2):e018557.
15. Wilson J, Jungner Y. Principles and Practice of Screening for Disease. Ann Intern Med. 1968 Nov 1; 69(5):1085.
16. Keeffe JE, Chou S-L, Lamoureux EL. The cost of care for people with impaired vision in Australia. Arch Ophthalmol. 2009 Oct; 127(10):1377–81.
17. Fricke T, Holden B, Wilson D, et al. Global cost of correcting vision impairment from uncorrected refractive error. Bull World Health Organ. 2012 Oct 1; 90(10):728–38.
18. WHO | Priority eye diseases. 2018 Apr 18 [cited 2019 Sep 2]; Available from: http://www.who.int/blindness/causes/priority/en/index4.html
19. Australia’s health 2014 (full publication; 21 Jul 2014 edition) (AIHW). Available from: http://www.aihw.gov.au/getmedia/d2946c3e-9b94-413c-898c-aa5219903b8c/16507.pdf.aspx?inline=true
20. Zloto et al. Current trends among pediatric ophthalmologists to decrease myopia progression—an international perspective. Graefes Arch Clin Exp Ophthalmol. 2018 Dec 1; 256(12):2457–66.
21. Wildsoet CF, Chia A, Cho P, et al. IMI - Interventions Myopia Institute: Interventions for Controlling Myopia Onset and Progression Report. Invest Ophthalmol Vis Sci. 2019 Feb 28; 60(3):M106–31.
22. Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017 Sep; 95(6):551–66.
23. Tran HDM, Tran YH, Tran TD, et al. A Review of Myopia Control with Atropine. J Ocul Pharmacol Ther. 2018 Jun; 34(5):374–9.
24. Vagge A, Ferro Desideri L, Nucci P, et al. Prevention of Progression in Myopia: A Systematic Review. Diseases. 2018 Sep 30; 6(4).
25. Gong Q, Janowski M, Luo M, et al. Efficacy and Adverse Effects of Atropine in Childhood Myopia: A Meta-analysis. JAMA Ophthalmol. 2017 Jun 1; 135(6):624–30.
26. Chia A, Lu Q-S, Tan D. Five-Year Clinical Trial on Atropine for the Treatment of Myopia 2: Myopia Control with Atropine 0.01% Eyedrops. Ophthalmology. 2016 Feb; 123(2):391–9.
27. Bullimore MA, Berntsen DA. Low-Dose Atropine for Myopia Control: Considering All the Data. JAMA Ophthalmol. 2018 Mar 1; 136(3):303.
28. Yam JC, Jiang Y, Tang SM, et al. Low-Concentration Atropine for Myopia Progression (LAMP) Study: A Randomized, Double-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. Ophthalmology. 2019 Jan; 126(1):113–24.
29. Wen D, Huang J, Chen H, Bao F, et al. Efficacy and Acceptability of Orthokeratology for Slowing Myopic Progression in Children: A Systematic Review and Meta-Analysis. J Ophthalmol. 2015 Jun 11; 2015:360806.
30. Myopia guidelines [Internet]. Brien Holden Vision Institute. [cited 2019 Sep 8]. Available from: www.brienholdenvision.org/translational-research/myopia/myopia-guidelines.html
31. Gifford KL, Richdale K, Kang P, et al. IMI - Clinical management guidelines report. Invest Ophthalmol Vis Sci. 2019 Feb 28; 60(3):M184–203.
32. Pharmaceutical Management Agency Section H Update for Hospital Pharmaceuticals Effective 1 August 2018. Pharmaceutical Management Agency; August 2018: 18.
33. Payerols A, Eliaou C, Trezeguet V, et al. Accuracy of PlusOptix A09 distance refraction in pediatric myopia and hyperopia. BMC Ophthalmol. 2016 Jun 1; 16:72.
34. Yu H, Shao Y, Yuan H, Yan B. Age-determined referral criteria of myopia for large-scale vision screening. Eye Sci. 2015 Dec; 30(4):151–5.
35. Ma Y, He X, Zou H, et al. Myopia screening: combining visual acuity and noncycloplegic autorefraction. Optom Vis Sci. 2013 Dec; 90(12):1479–85.
36. Fogel-Levin M, Doron R, Wygnanski-Jaffe T, et al. A comparison of plusoptiX A12 measurements with cycloplegic refraction. J AAPOS. 2016 Aug; 20(4):310–4.
37. Cumberland PM, Bountziouka V, Rahi JS. Impact of varying the definition of myopia on estimates of prevalence and associations with risk factors: time for an approach that serves research, practice and policy. Br J Ophthalmol. 2018; 102(10):1407–12.
38. Dirani M, Shekar SN, Baird PN. Evidence of Shared Genes in Refraction and Axial Length: The Genes in Myopia (GEM) Twin Study [Internet]. Vol. 49, Investigative Opthalmology & Visual Science. 2008. p. 4336. Available from: http://dx.doi.org/10.1167/iovs.07-1516
39. Yu L, Li Z-K, Gao J-R, et al. Epidemiology, genetics and treatments for myopia. Int J Ophthalmol. 2011 Dec 18;4(6):658–69.
40. Bock GR, Widdows K. Myopia and the control of eye growth. John Wiley & Sons; 2008. 266 p.
41. Zhang S, Yang J, Reinach PS, et al. Dopamine receptor subtypes mediate opposing effects on form deprivation myopia in pigmented guinea pigs. Invest Ophthalmol Vis Sci. 2018 Sep 4; 59(11):4441–8.
42. Frick KD, Gower EW, Kempen JH, Wolff JL. Economic impact of visual impairment and blindness in the United States. Arch Ophthalmol. 2007 Apr; 125(4):544–50.
43. Zheng Y-F, Pan C-W, Chay J, et al. The economic cost of myopia in adults aged over 40 years in Singapore. Invest Ophthalmol Vis Sci. 2013 Nov 13; 54(12):7532–7.
