ARTICLE
Vol. 133 No. 1509 |
Ethnic inequities in life expectancy attributable to smoking
There are large and persistent inequities in mortality and life expectancy among Māori and Pacific when compared with non-Māori/non-Pacific people, in New Zealand.
Full article available to subscribers
There are large and persistent inequities in mortality and life expectancy among Māori and Pacific when compared with non-Māori/non-Pacific people, in New Zealand. Life expectancy at birth, an easily understandable summary measure of population health, is reflective of current mortality across different age groups and allows comparison of groups with different population structures. In 2013–15, life expectancy differentials were approximately seven years for Māori (6.8 years in women, 7.3 years in men) and more than five years for Pacific peoples (5.2 years in women, 5.8 years in men) when compared to the non-Māori/non-Pacific population.1
Smoking is recognised as one of the most significant risk factors contributing to non-communicable diseases.2 It is strongly linked to lung cancer and confers increased risk of death from other cancers, heart disease, stroke, chronic respiratory disease and a number of other conditions.3 Tobacco smoking in New Zealand has previously been estimated to result in the deaths of between 4,500 and 5,000 individuals per year.4
Although the daily smoking prevalence in New Zealand adults has steadily declined,5 an ethnic gradient exists, with the prevalence of smoking nearly three times higher among Māori and one and a half times higher among Pacific compared with non-Māori/non-Pacific people. Despite a declining prevalence of the past 10 years, the prevalence for Māori women remains persistently higher than Māori men (35% vs 27%). Trends for Pacific men and women have not changed significantly between 2006/07 and 2017/18 and are higher in men compared to women (25% vs 15%). More recently, some of the largest total population declines have occurred among the 15–34 year age group, particularly among those aged 15–17 years. This suggests that declining initiation rates in youth are contributing towards a reduction in smoking prevalence.
Consistent with persistent disparities in smoking prevalence, Māori and Pacific peoples are disproportionately burdened by smoking-related morbidity and mortality.6 There is a large body of evidence indicating that tobacco is likely the leading contributor to health inequities among Māori and Pacific populations,7–9 reflecting the unfair and unjust distribution of social, environmental and economic determinants of health. Both Māori and non-Māori current-smokers have been shown to have a lower life expectancy compared with non-smokers. The gap between current- and never-smokers, however, is smaller among Māori than among non-Māori (4.3 and 3.9 years among Māori men and women respectively, compared to 7.4 and 6.2 years among non-Māori) and has been attributed to the much higher background mortality among Māori never-smokers compared to non-Māori never-smokers.10
Understanding the impact of tobacco smoking and the contribution to ethnic inequities is necessary to inform policies and strategies for fair and just tobacco control as well as health service planning. In this study we use recent mortality and smoking prevalence data to provide updated estimates of its contribution to all-cause mortality, and of smoking-related mortality to the life expectancy gap in both Māori and Pacific ethnic groups compared with non-Māori/non-Pacific ethnic groups in New Zealand. We also decompose the life expectancy gap by specific smoking attributable causes of death.
Method
Smoking prevalence
Age-, ethnic- and sex-specific smoking prevalence was calculated using total response data from the 2013 Census.11 Ethnicity in New Zealand is self-identified. Multiple ethnicities were prioritised to Māori, Pacific, Asian and European/Other as per standard protocols for health research.12
Estimating the number of smoking attributable deaths
We applied population-attributable fraction (PAF) methods that combine summary measures of prevalence, relative risk and mortality.13 Population-attributable fraction estimates the proportion of disease that can be attributed to a particular risk factor. PAF is derived mathematically by combining the prevalence of the risk factor (Pc—current smokers and Pf—ex-smokers) in the target population with a measure of association between the risk factor and burden (Rc—current smokers, Rf—ex-smokers), obtained from epidemiological studies.
Consistent with previous international studies of smoking related mortality, we used the American Cancer Society Cancer Prevention Study II (CPS-II) relative risk estimates for smoking related diseases (Table 1).14 The CPS-II is an ongoing prospective study of 1,185,106 residents in the US, aged 30 years or over, for those who, in 1982, had never smoked regularly, and for those who were then current cigarette smokers. The use of relative risk estimates from international studies has previously been used to describe the burden of smoking-related disease in New Zealand.15–17 In many ways the CPS-II estimates have unofficially taken the role of being the “gold standard” for the effect measure in estimating smoking attributable mortality.
Using the applicable ICD10 codes for identified smoking-related diseases, smoking attributable fractions for each disease casually linked to smoking were calculated using the following formula for multiple exposure groups:
· PAF is the attributable proportion for each disease attributable to smoking
· Pc is the proportion of the population who are current smokers
· Pf is the proportion of the population who are ex-smokers
· Rc is the disease specific relative risk of death for current smokers
· Rf is the disease specific relative risk of death for ex-smokers
The age-, sex- and ethnic-specific PAF for each cause were multiplied by the number of deaths in the population from each respective cause to obtain cause-specific smoking-attributable mortality estimates. For each cause of death group, smoking-attributable mortality estimates were calculated for men and women, for each ethnic group and either for all age groups or by the four age groups 35–54, 55–64, 65–74 and 75+ years if age-specific relative risk estimates were available. The proportion of smoking attributable deaths was summed to generate the total number of deaths attributable to smoking. Our estimates of smoking attributable mortality do not take into account deaths attributable to second-hand smoke or occupational exposure.
Decomposition of life expectancy
Life expectancy at birth using data for 2013–15 (three year aggregated) was calculated using standard abridged life table techniques, with 90 and older being the final age group. The impact of smoking on the differentials in life expectancy was estimated by decomposing the difference in life expectancy using the method developed by Arriaga.18 This method allows differentials in life expectancy to be decomposed into age group and cause-of-death-specific contributions. Each sums to the total differential in life expectancy between groups. Both the total sum of smoking attributable mortality and cause specific smoking attributable mortality were decomposed.
Life tables for Māori men, Māori women, Pacific men, Pacific women, non-Māori/non-Pacific men and non-Māori/non-Pacific women were developed. The sex-specific non-Māori/non-Pacific tables served as the comparator group for the Māori and Pacific sex-specific tables. The contribution of smoking attributable mortality on life expectancy differentials in both Māori and Pacific compared with non-Māori/non-Pacific was analysed. The gap in life expectancy was decomposed both by the sum of all smoking attributable deaths and by the sum of smoking attributable deaths by specific cause.
Results
Total smoking attributable deaths
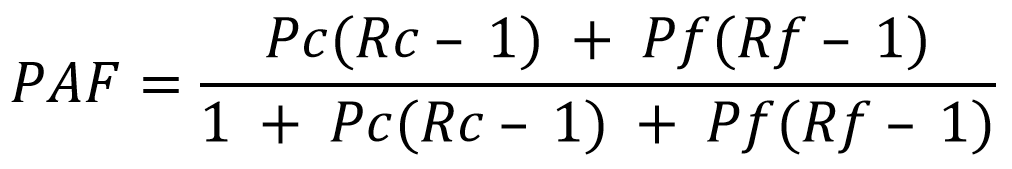
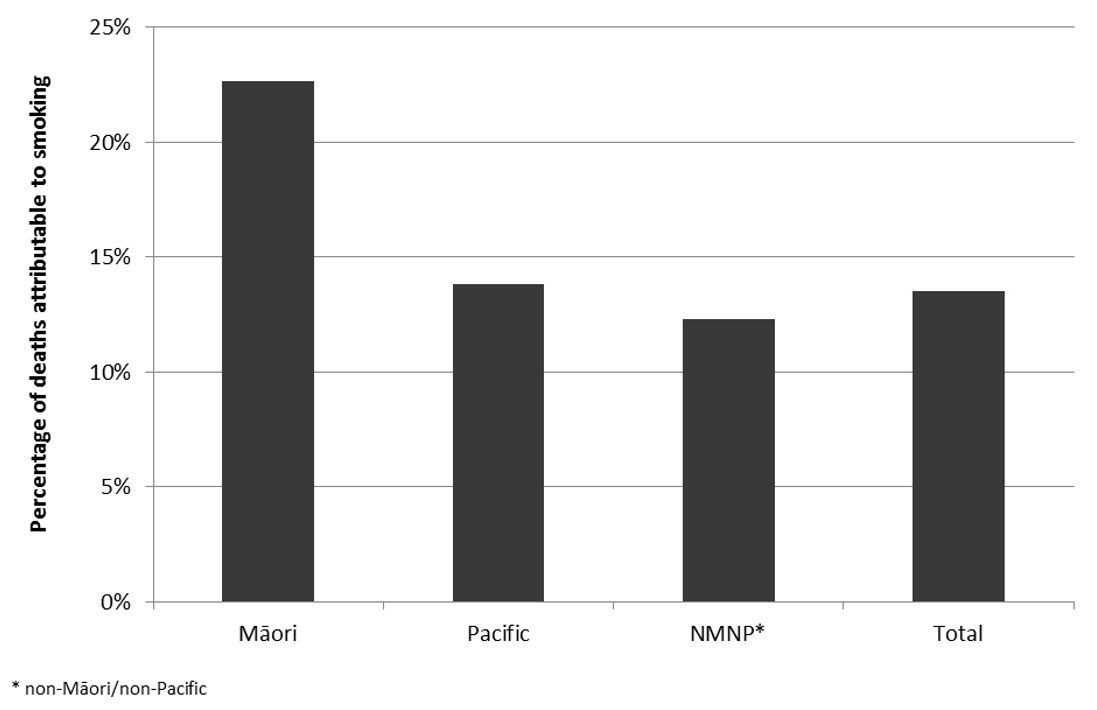
Between 2013 and 2015 there were 92,196 deaths registered in New Zealand. Of these deaths we estimated that 12,421 (13.4% of all deaths) or nearly one in seven were attributable to smoking. The proportion of smoking attributable deaths varied by ethnicity (Figure 1) with nearly one in four (22.6%) deaths among Māori attributable to smoking (2,199 out of 9,717 deaths) and nearly one in seven (13.8%) among Pacific People (512 out of 3,720 deaths). Among non-Māori/non-Pacific people one in eight (12.3%) deaths were attributable to smoking (9,710 out of 78,759).
Figure 1: Percentage of deaths attributable to smoking by ethnicity, 2013–2015.
Overall, 30.7% of smoking attributable deaths were from trachea, bronchus and lung cancers followed by COPD (26.0%) and ischaemic heart disease (13.2%). Among Māori 37.5% of smoking attributable deaths were from trachea, bronchus and lung cancers compared with 29.5% in Pacific.
Life expectancy at birth
For all deaths registered in 2013–15, estimates of life expectancy were: 73.5 years in Māori men, 77.3 years in Māori women, 75.0 years in Pacific men and 78.3 years in Pacific women. In comparison, life expectancy was 80.9 years in non-Māori/non-Pacific men and 84.3 years in non-Māori/non-Pacific women. These results equated to differentials in life expectancy of 7.4 years in Māori men, 7.0 years in Māori women, 5.9 years in Pacific men, and 6.0 years in Pacific women.
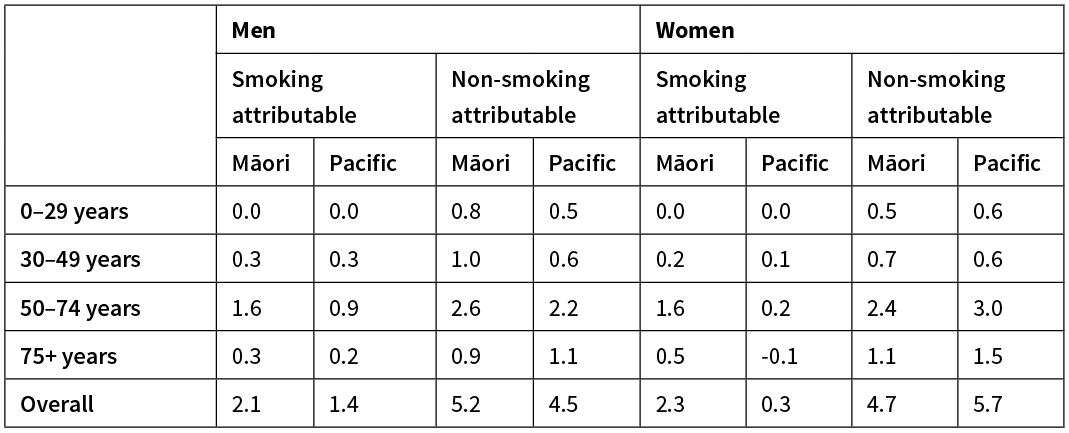
Contribution of smoking to the life expectancy gap—Māori
Among Māori men, 2.1 years (28.4%) of the 7.4 year gap in life expectancy was attributable to the higher mortality rates from smoking attributable deaths. Among Māori women, the contribution from smoking attributable deaths was 2.3 years (32.9%) of the 7.0 year gap (Table 1).
Table 1: Contribution of smoking attributable mortality to the life expectancy gap, 2013–15.
The leading smoking attributable causes of death contributing to the life expectancy gap were cancers of the trachea, bronchus and lung, contributing nearly one full year to the gap among Māori women (Figure 2) and 0.8 years among Māori men (Figure 3). This was followed in Māori men by smoking attributable ischaemic heart disease (0.5 years of the gap) and COPD (0.3 years of the gap). Among Māori women COPD was the second leading smoking attributable cause of death (0.5 years of the gap) followed by smoking attributable ischaemic heart disease (0.3 years of the gap).
Figure 2: Decomposition of the life expectancy gap by smoking attributable cause—Māori women.
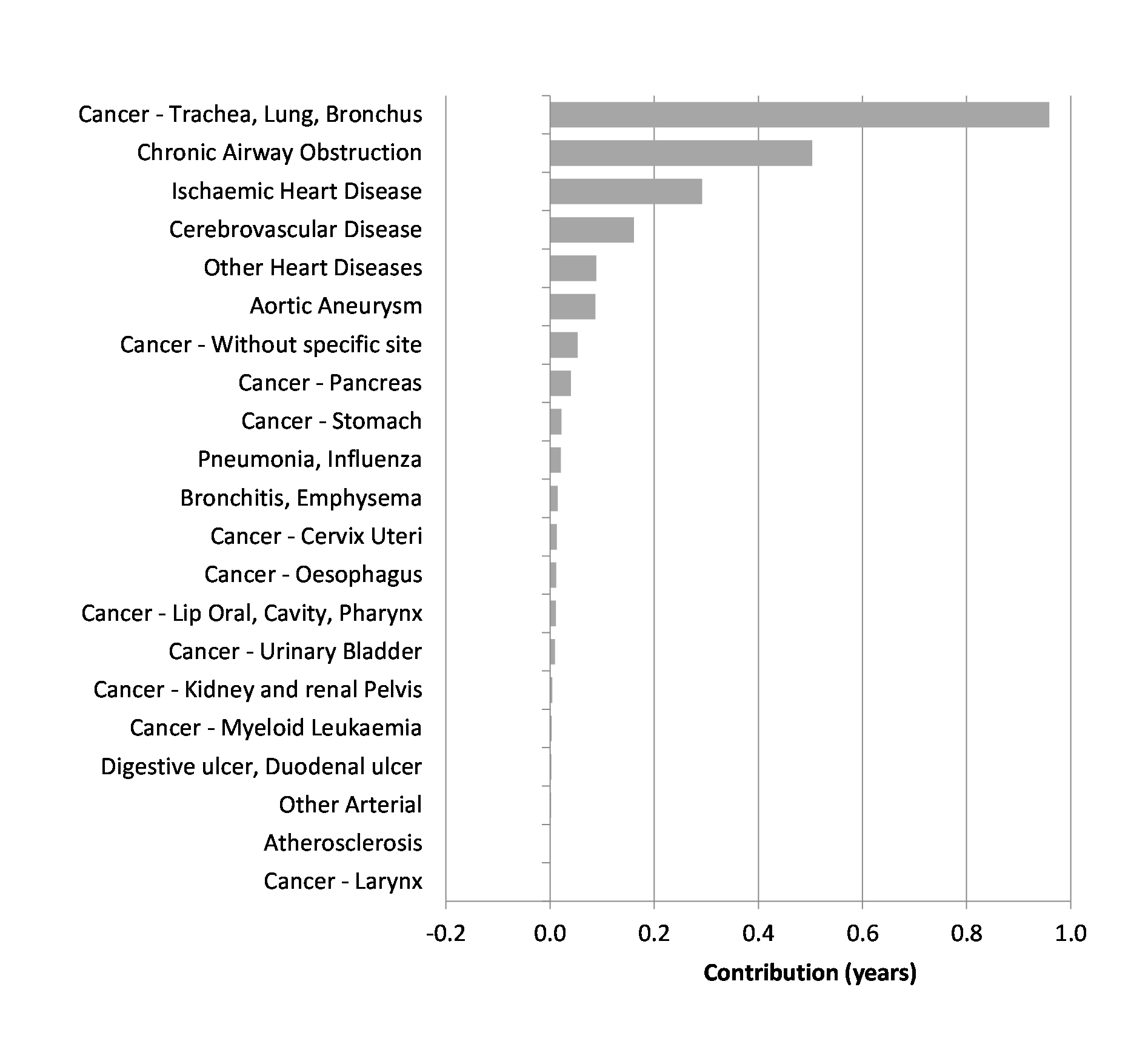
Figure 3: Decomposition of the life expectancy gap by smoking attributable cause—Māori men.
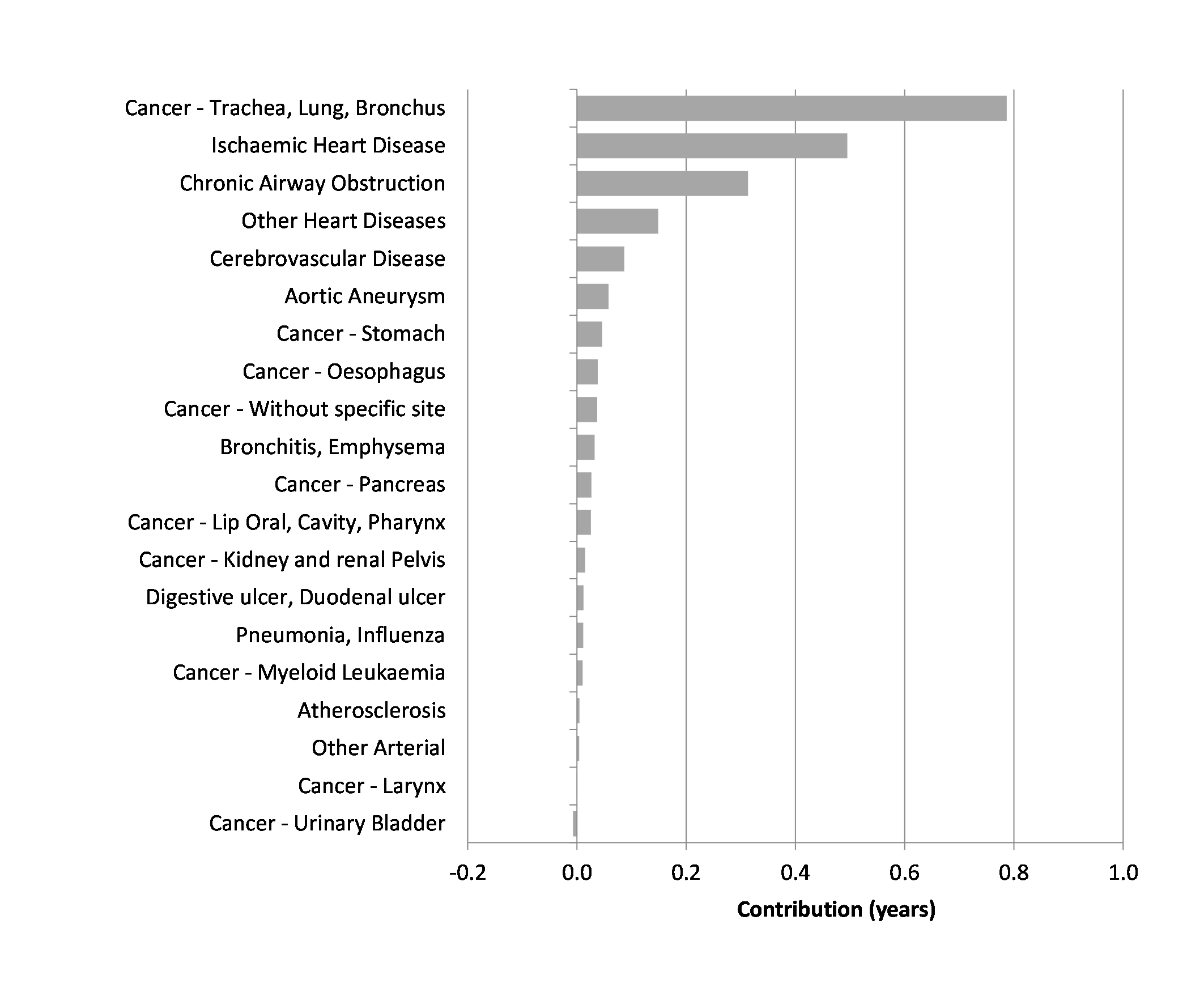
Figure 4: Decomposition of the life expectancy gap by smoking attributable cause—Pacific men.
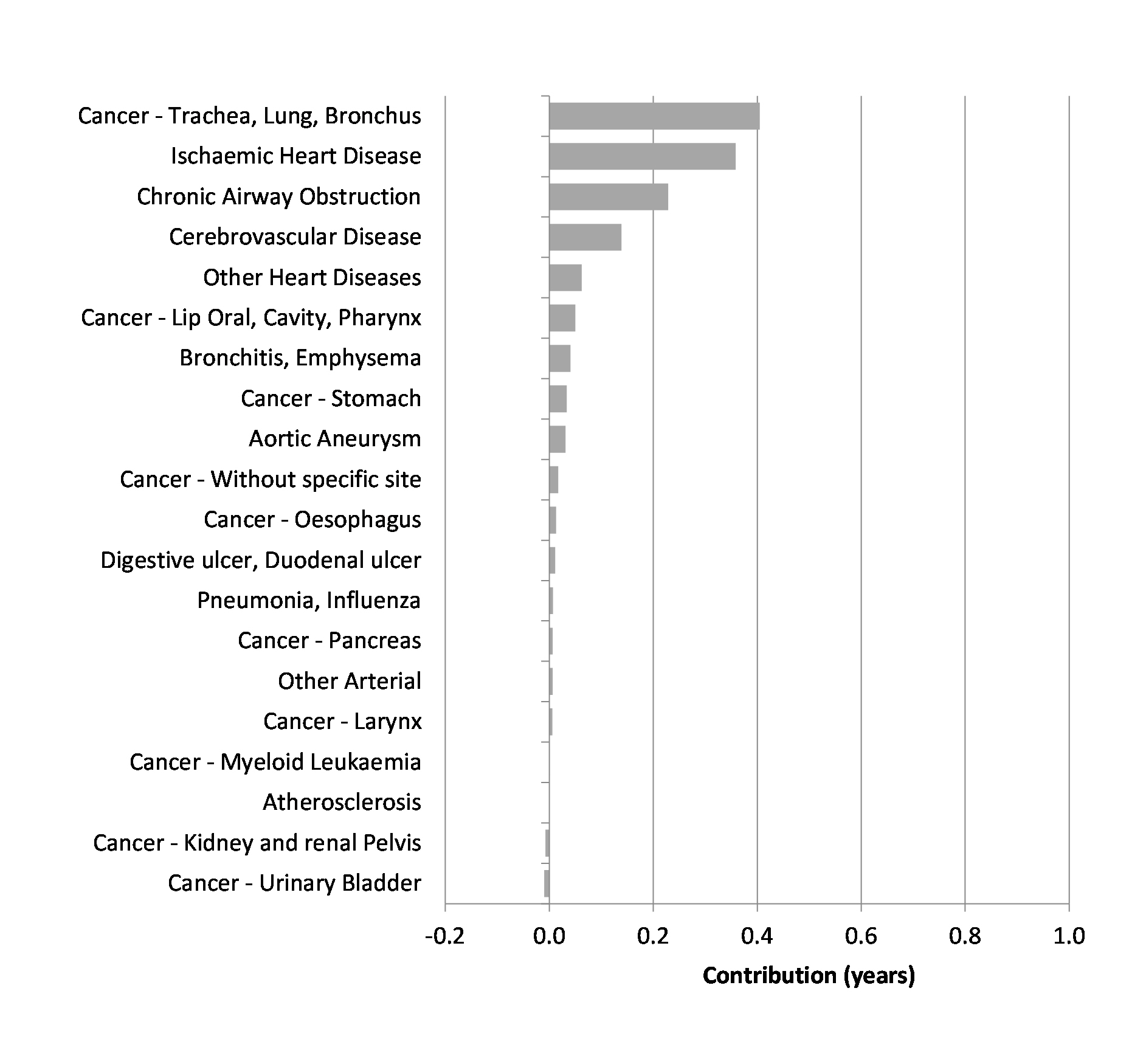
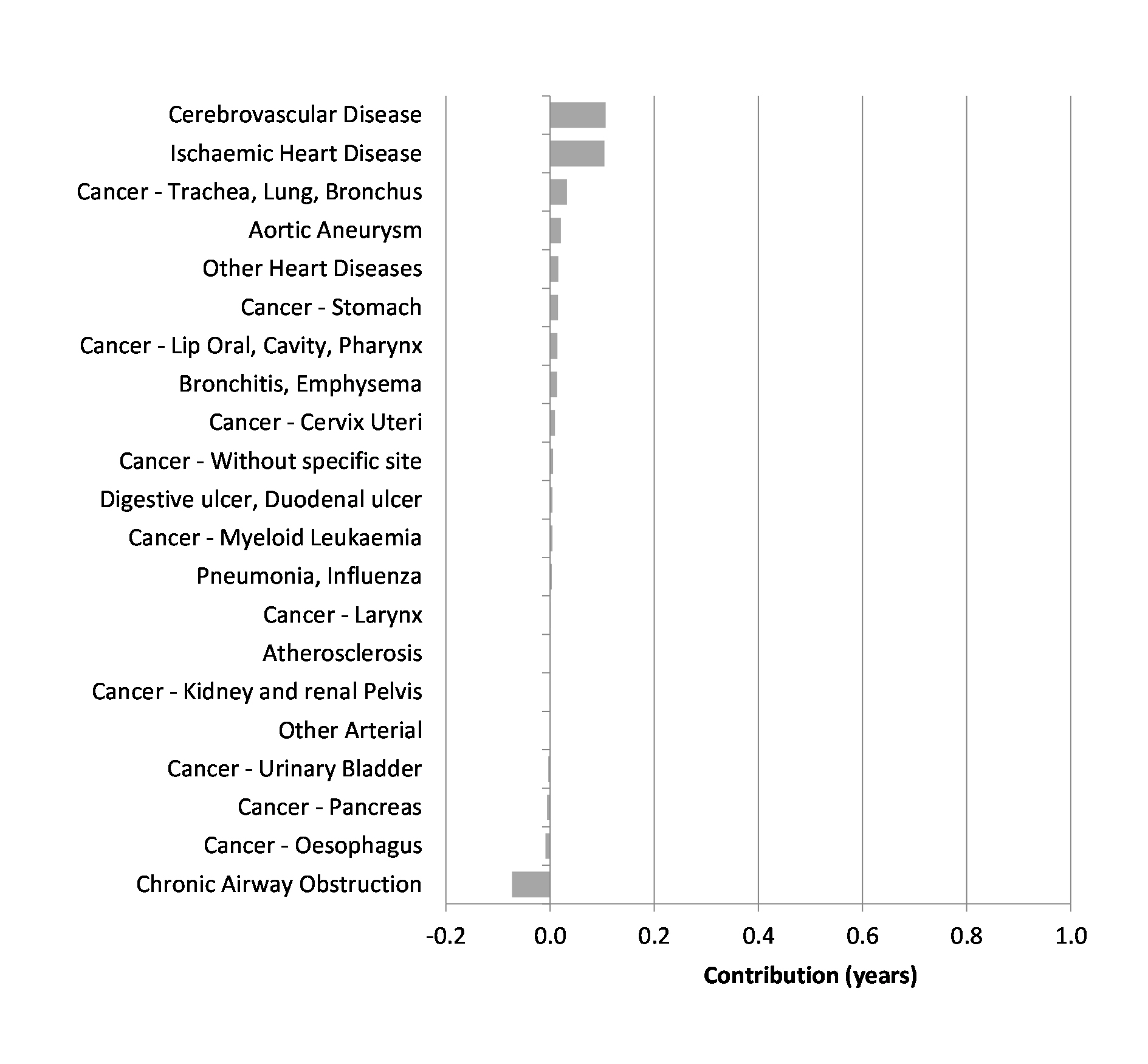
Figure 5: Decomposition of the life expectancy gap by smoking attributable cause—Pacific women.
Contribution of smoking to the life expectancy gap—Pacific
Among Pacific men 1.4 years (23.7%) of the 5.9 year gap in life expectancy was attributable to the higher mortality rates from smoking attributable causes of death. Among Pacific women, the contribution from smoking attributable causes of death was 0.3 years (5.0%) of the 6.0 year gap (Table 1).
The leading smoking attributable causes of death among Pacific men contributing to the life expectancy gap were cancers of the trachea, bronchus and lung and ischaemic heart disease, each contributing 0.4 years to the life expectancy gap (Figure 4), followed by smoking attributable COPD (0.2 years of the gap). In Pacific women cerebrovascular disease and ischaemic heart disease were the leading smoking attributable causes of death, each contributing 0.1 years to the gap (Figure 5).
Discussion
Our study provides an updated assessment of the burden of smoking-related mortality in New Zealand for deaths registered from 2013 to 2015 and examines the contribution of these deaths to the life expectancy gap in the Māori and Pacific populations compared with the non-Māori/non-Pacific population. Over this time, 13.4% of deaths were potentially attributable to smoking. Among Māori, 22.6% of deaths were potentially attributable to smoking, compared with 13.8% of deaths among Pacific peoples and 12.3% among non-Māori/non-Pacific people. We estimate that smoking attributable deaths contributed 2.1 years to the life expectancy gap in Māori men, 2.3 years in Māori women, 1.4 years of Pacific men and 0.3 years in Pacific women.
Smoking attributable deaths and the contribution to inequities in life expectancy have been previously described, albeit using differing methods. For the period 1996–1999, Blakely et al found that current smokers had an estimated 3.9–7.4 years less of life expectancy relative to never-smokers.10 The smoking attributable difference in life expectancy was smaller among Māori than among non-Māori. The Ministry of Health has also estimated the burden of smoking using similar methods to this study to estimate the number of smoking attributable deaths and the contribution of smoking to ethnic inequities in life expectancy.15 Using the life expectancy of the Europeans in the lowest level of deprivation (most socioeconomically advantaged) with smoking deaths removed as a comparator, the report showed that 3.5 years of the life expectancy gap in Māori men and 2.4 years in Māori women was attributable to tobacco. Among Pacific peoples this gap was 3.6 years in men and 0.9 years in women. The contributions of tobacco in both studies were larger than those we present. This difference is primarily due to the reference group used. In the prior studies, the reference group was either life expectancy with the smoking attributable deaths removed or the life expectancy of never smokers. The reference group used in our study was the non-Māori/non-Pacific population without smoking deaths removed. As such, our estimates account for the smoking attributable deaths in the non-Māori/non-Pacific population and can be interpreted as the gap in life expectancy due to the difference in smoking attributable deaths in the Māori and Pacific populations compared with the non-Māori/non-Pacific population.
We found a smaller contribution of smoking to the life expectancy gap in Pacific men (1.4 years) and women (0.3 years) compared to Māori. This likely reflects the lower prevalence of smoking overall, lower prevalence in older age groups and that Pacific people are less likely to be daily smokers when compared with Māori.5 For Māori the additional burden of smoking attributable mortality could be a result of a greater intensity of exposure to second-hand smoke when compared to other ethnicities. This likely comes about as a result of the higher density of Māori who smoke both at home and in the workplace.19 Another explanation is that other risk factors, such as excess body weight, are potentially greater contributors to mortality and the life expectancy gap among the Pacific population. It has been previously shown that diseases related to excess body weight, such as diabetes and uterine cancers, are among the leading contributors to the life expectancy gap among the Pacific population.1
Drivers of inequity
Factors contributing to the pervasive and persisting ethnic health inequities are multifaceted and complex. Three main pathways have been identified: (i) differential access to the determinants of health or exposures leading to differences in disease incidence, (ii) differential access to healthcare and (iii) differences in quality of care received.20 These pathways are driven by different levels of racism, particularly institutionalised and personally mediated or interpersonal racism.21
Similar to other indigenous populations, the colonisation of New Zealand severely impacted Māori and resulted in social marginalisation and poor health outcomes through the redistribution of Māori power and resources.22 Historical and ongoing colonisation processes have led to the unequal distribution of resources, such as education, employment and income, which shape exposure to risk factors, such as smoking, for potentially avoidable diseases and mortality. In addition, tobacco was a common trade commodity between Māori and non-Māori in the 1800s, contributing towards widespread uptake among Māori.23
Persisting and pervasive health inequities are a breach of Te Tiriti o Waitangi. The recent Waitangi Tribunal Report on Stage One of the Health Service and Outcomes Kaupapa Inquiry identified Tiriti non-compliance across multiple areas of primary healthcare and systems that are relevant to smoking and smoking-related burden of disease in Māori.24 Tobacco is also a focus area in stage two of the Waitangi Tribunal Health Services and Outcomes Inquiry. The inquiry will hear claims concerning grievances relating to health services and outcomes of national significance.25
Smokefree 2025
In 2011 the Government adopted the Smokefree Aotearoa 2025 goal in response to the landmark Parliamentary inquiry by the Māori Affairs Select Committee.26 The goal aspires to achieve a daily smoking prevalence of less than five percent by 2025. Although wide-ranging interventions have been introduced since 2011 (including tobacco taxation, cessation support, mass media campaigns, smoke free environment legislation, and plain packaging and health warnings), a national strategy for achieving Smokefree Aotearoa is absent.
A business-as-usual approach to tobacco control is insufficient to meet the needs of Māori and Pacific peoples. Current trends, along with modelling studies, suggest that New Zealand is unlikely to meet its Smokefree 2025 goal and will likely be substantially missed for Māori.27 Wilson et al projected smoking prevalence rates in 2025 to be 17.4% for Māori and 7.2% for non-Māori. The authors suggest that to achieve the New Zealand Government’s Smokefree 2025 Goal, there would need to be an additional 8,400 Māori long-term quitters per year—more than five times the current annual level. Even for non-Māori, quit rates would need to double. Wilson et al state that reaching the 2025 goal would require significantly enhanced investment in established smoking cessation services and mass media campaigns or the addition of substantive novel interventions.
Long-term residual risk in ex-smokers
Following cessation, ex-smokers carry a disease-specific residual risk of between 10 and 40 years.28 Subsequently, the life expectancy gap as a result of smoking attributable diseases will likely persist for some time. For the leading smoking attributable condition, lung cancer, the downturn in risk occurs faster in women than men. The risk in men returns to that of never-smokers at around 40 years following cessation, whereas in women this occurs between 25 to 30 years following cessation. COPD has the slowest decline in risk in the first 25 years after cessation, whereas cardiovascular disease has the most rapid reduction. After about 10 years of smoking cessation, the risk of dying from cardiovascular disease in ex-smokers is approximately equal to that of never-smokers.28
With the residual risk that ex-smokers continue to carry for many years following cessation, an important component of reducing smoking attributable mortality, and thus the life expectancy gap attributable to smoking, will be managing this risk in ex-smokers. Given that the prevalence of smoking still remains high for Māori men and women and Pacific men, and that patterns of disease incidence largely reflect historical smoking patterns,29 it is likely that differences in smoking attributable mortality and thus the life expectancy gap attributable to smoking will persist for some time.
Strengths and limitations
Our study has several strengths. First we used national mortality data that achieves nearly complete coverage of the New Zealand population. With a well-established mortality data collection system we had access to precise numbers of ethnic, gender and cause-specific death information for PAF estimation. Second, the relative risk estimates in our study were derived from a very large-scale population-based cohort study with over 1.1 million subjects, giving reliable relative risk estimates. Third, the smoking prevalence was obtained from national census data. The Census has the advantage of reaching between 93–95% of the New Zealand adult population (aged 15+), and, as it is a census of the total population, is not subject to sampling error. However, post-enumeration surveys show that there is likely to be an undercounting of people who smoke, since Māori and Pacific peoples are over-represented in the groups most likely to be missed by the Census.
PAF methods are a useful way to theoretically quantify the burden of a particular risk factor. However, they are based on assumptions that include some level of uncertainty and likely resulted in underestimating the smoking attributable fractions and thus the number of smoking attributable deaths. Many of the issues and limitations of PAF methods stem from using and combining ecological, summary measures of exposure, outcome and relative risk, across different sources of data. Firstly, exposure mismatch can occur where the definition of exposure categories (eg, current and former smoking) across data-sources for prevalence and relative risk differ. In addition, temporal changes in smoking prevalence and in accumulation/reversibility of disease-specific risks are not accounted for, along with deaths from second-hand smoke exposure. Second, external generalisability and heterogeneity of the selected relative risk estimates due to exposure definitions and distributions between the study source and usage in this study. It is plausible that the strength of the association varies in New Zealand and may also vary by ethnic group due to different baseline risks. To the best of our knowledge no single study has been able to provide disease-specific smoking-related risk estimates for New Zealand; as such the numbers from CPS-II should only be considered an approximation.30
Finally, the distribution of potential confounders in the population of interest has not been accounted for as individual-level adjustment is not possible. We have also not explicitly allowed for passive/second-hand smoking. This most probably affects more Māori than non-Māori.31 As a result, we have likely further underestimated the full impact of smoking on ethnic gaps in life expectancy attributable to smoking. Despite these limitations, the estimates provide policymakers and the public with a general understanding of the magnitude of the burden imposed on the nation, and in particular Māori and Pacific peoples, by smoking.
Conclusion
A significant proportion of the life expectancy gap for Māori men and women and Pacific men is a result of smoking attributable deaths. Addressing this inequity needs to remain a top health priority. In order to achieve health equity and the Smokefree 2025 goal, a Tiriti o Waitangi compliant response inclusive of targeted investment and expansion of Māori and Pacific tobacco control programmes is required. Should New Zealand be successful in achieving its smokefree goal, addressing the residual risk in ex-smokers through equitable early diagnosis and treatment of smoking-related morbidity, will reduce the number of smoking attributable deaths and more rapidly close the life expectancy gap, particularly for Māori. History demonstrates that without deliberate attention and commitment to achieving equitable health outcomes for Māori and Pacific peoples they will not be achieved. The next five years provide an opportunity to demonstrate commitment to achieving a smoke-free Aotearoa for all, an aspiration, based on the current trajectory, which is most probably out of reach.
Aim
To determine the contribution of smoking-related deaths to the life expectancy gap in both Māori and Pacific people compared with non-Māori/non-Pacific people in New Zealand.
Methods
Death registration and population data between 2013 and 2015 were used to calculate life expectancy. To determine the contribution of smoking to the life expectancy gap, population attributable fractions for all causes of death where smoking is a casual risk factor were calculated using age- and ethnic-specific smoking data from the 2013 New Zealand Census and relative risk estimates from the American Cancer Society Cancer Prevention Study II. Population attributable fractions were applied to all deaths registered in New Zealand for the 2013–15 period to estimate the number of deaths attributable to tobacco smoking. The life expectancy gap was decomposed using the Arriaga method. The gap was decomposed both overall and by specific smoking attributable causes of death.
Results
Between 2013 and 2015 an estimated 12,421 (13.4% of all deaths) were attributable to smoking. Nearly one in four (22.6%) deaths among Māori were attributable to smoking (2,199 out of 9,717 deaths) and nearly one in seven (13.8%) among Pacific people (512 out of 3,720 deaths). Among non-Māori/non-Pacific people, one in eight (12.3%) deaths were attributable to smoking (9,710 out of 78,759 deaths). Higher rates of smoking attributable mortality were responsible for 2.1 years of the life expectancy gap in Māori men, 2.3 years in Māori women, 1.4 years in Pacific men and 0.3 years among Pacific women. Cancers of the trachea, bronchus and lung, chronic obstructive pulmonary disease (COPD) and ischaemic heart disease were the leading smoking attributable causes of death contributing to the gap.
Conclusion
Smoking is an important preventable risk factor contributing to ethnic inequities in life expectancy for Māori men and women, and Pacific men. Dramatic declines in smoking-attributable deaths can be achieved by reducing smoking prevalence rates. Preventing smoking initiation and increasing cessation rates must remain a top priority for the Ministry of Health and District Health Boards. Smokefree initiatives should be reoriented to be Tiriti o Waitangi (Treaty of Waitangi) compliant and better meet the needs of Māori and Pacific people who smoke. Addressing the residual risk in ex-smokers through equitable early diagnosis and treatment of smoking-related conditions will further assist a more rapid closing of life expectancy gaps for Māori men and women and Pacific men. The next five years provide the opportunity to demonstrate commitment to achieving a smokefree Aotearoa for all: an aspiration, based on the current trajectory, which is most probably out of reach.
Authors
Michael Walsh, Epidemiologist, Planning Funding and Outcomes, Waitemata District Health Board, Auckland; Karen Wright, Public Health Registrar, Planning Funding and Outcomes, Waitemata District Health Board, Auckland.Correspondence
Michael Walsh, Planning Funding and Outcomes, Waitemata District Health Board, Level 1, 15 Shea Terrace, Takapuna, Auckland.Correspondence email
michael.walsh@waitematadhb.govt.nzCompeting interests
Nil.1. Walsh M, Grey C. The contribution of avoidable mortality to the life expectancy gap in Māori and Pacific populations in New Zealand-a decomposition analysis. N Z Med J. 2019; 132:46–60.
2. Kontis V, Mathers CD, Rehm J, et al. Contribution of six risk factors to achieving the 25x25 non-communicable disease mortality reduction target: a modelling study. Lancet. 2014; 384:427–37.
3. U.S. Department of Health and Human Services. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2014.
4. Ministry of Health. Tobacco Trends 2008: A brief update of tobacco use in New Zealand. Wellington: Ministry of Health; 2009.
5. Ministry of Health. Annual Data Explorer 2017/18: New Zealand Health Survey [Data File]. [cited]. Available from: http://minhealthnz.shinyapps.io/nz-health-survey-2017-18-annual-data-explorer
6. Ministry of Health. The burden of disease and injury in New Zealand. Public Health Intelligence Occasional Bulletin No.1. Wellington: Ministry of Health; 2001.
7. Blakely T, Fawcett J, Hunt D, et al. What is the contribution of smoking and socioeconomic position to ethnic inequalities in mortality in New Zealand? Lancet. 2006; 368:44–52.
8. Blakely T, Disney G, Valeri L, et al. Socioeconomic and Tobacco Mediation of Ethnic Inequalities in Mortality over Time: Repeated Census-mortality Cohort Studies, 1981–2011. Epidemiology. 2018; 29:506–16.
9. Wilson N, Blakely T, Tobias M. What potential has tobacco control for reducing health inequalities? The New Zealand situation. Int J Equity Health. 2006; 5:14.
10. Blakely T, Carter K, Wilson N, et al. If nobody smoked tobacco in New Zealand from 2020 onwards, what effect would this have on ethnic inequalities in life expectancy? N Z Med J. 2010; 123:26–36.
11. Statistics New Zealand. Census 2013, cigarette smoking behaviour and ethnic group (DHB) [Customised data request]. 2013.
12. Ministry of Health. HISO 10001:2017 Ethnicity Data Protocols. [cited 1/08/2019]. Available from: http://www.health.govt.nz/system/files/documents/publications/hiso-10001-2017-ethnicity-data-protocols.pdf
13. Hanley JA. A heuristic approach to the formulas for population attributable fraction. J Epidemiol Community Health. 2001; 55:508–14.
14. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA), 2014.
15. Ministry of Health. Inhaling inequality. Tobacco’s contribution to health inequality in New Zealand. Wellington: Ministry of Health; 2001.
16. Blakely T, Cobiac LJ, Cleghorn CL, et al. Health, Health Inequality, and Cost Impacts of Annual Increases in Tobacco Tax: Multistate Life Table Modeling in New Zealand. PLoS Med. 2015; 12:e1001856.
17. Ministry of Health. Health Loss in New Zealand 1990–2013: A report from the New Zealand Burden of Diseases, Injuries and Risk Factors Study. Wellington: Ministry of Health, 2016.
18. Arriaga EE. Measuring and explaining the change in life expectancies. Demography. 1984; 21:83–96.
19. Gillespie J, Milne K, Wilson N. Secondhand smoke in New Zealand homes and cars: exposure, attitudes, and behaviours in 2004. N Z Med J. 2005; 118:U1782.
20. Reid P, Robson B. Understanding Health Inequities. Hauora: Māori Standards of Health IV A study of the years 2000–2005. Wellington: Te Rōpū Rangahau Hauora a Eru Pōmare, 2007.
21. Jones CP. Invited commentary: “race,” racism, and the practice of epidemiology. Am J Epidemiol. 2001; 154:299–304; discussion 5–6.
22. Anderson I, Crengle S, Kamaka ML, et al. Indigenous health in Australia, New Zealand, and the Pacific. Lancet. 2006; 367:1775–85.
23. Reid R, Pouwhare R. Te Taonga Mai Tawhiti: The gift from a distant place. Auckland: Niho Taniwha, 1991.
24. Hauora - Report on Stage One of the Health Services and Outcomes Kaupapa Inquiry (WAI2575). Wellington, New Zealand: The Waitangi Tribunal, 2019.
25. Health Services and Outcomes Inquiry. [cited 19 July 2019]. Available from: http://www.waitangitribunal.govt.nz/inquiries/kaupapa-inquiries/health-services-and-outcomes-inquiry/
26. New Zealand Parliament. Inquiry into the tobacco industry in Aotearoa and the consequences of tobacco use for Māori, Report of the Māori Affairs Committee. Wellington: New Zealand Parliament, 2010.
27. Wilson N, Petrovic-van der Deen FS, Edwards R, et al. Modelling the number of quitters needed to achieve New Zealand’s Smokefree 2025 goal for Māori and non- Māori. N Z Med J. 2018; 131:30–7.
28. Oza S, Thun MJ, Henley SJ, et al. How many deaths are attributable to smoking in the United States? Comparison of methods for estimating smoking-attributable mortality when smoking prevalence changes. Prev Med. 2011; 52:428–33.
29. Shaw C, Blakely T, Sarfati D, et al. Varying evolution of the New Zealand lung cancer epidemic by ethnicity and socioeconomic position (1981–1999). N Z Med J. 2005; 118:U1411.
30. Hunt D, Blakely T, Woodward A, et al. The smoking-mortality association varies over time and by ethnicity in New Zealand. Int J Epidemiol. 2005; 34:1020–8.
31. Mason K. Burden of disease from second-hand smoke exposure in New Zealand. N Z Med J. 2016; 129:16–25.
