VIEWPOINT
Vol. 133 No. 1509 |
Nutrition guidelines for dental care vs the evidence: is there a disconnect?
Dental caries is the most common chronic childhood disease in New Zealand.
Full article available to subscribers
Dental caries is the most common chronic childhood disease in New Zealand.1 The most recent data from the Ministry of Health (MOH) showed that 40.5% of five-year-old children were diagnosed with dental caries in 2017, with a higher prevalence observed among Māori and Pacific children compared to children of other ethnicities. In addition, New Zealand is experiencing an obesity epidemic; New Zealanders are the third most overweight and obese population among countries included in the OECD.2 Approximately 67% of all New Zealanders over 15 years of age are overweight and the prevalence of obesity is 27%.1
There is now increasing scientific and public health debate that the common dietary behaviour—the high frequency consumption of sugar and starches and a concurrent reduced intake of nutrient-rich whole foods—is central to the development of dental caries, malnutrition in young children3 and obesity in older children.4 It is proposed that the consumption of ultra-processed sugars and starches leads to increased insulin secretion and dysregulation of the satiety hormone leptin, resulting in a cycle of increased hunger and frequent food consumption that promotes weight gain.5 MOH-endorsed dietary guidelines for healthy eating in children and young people in New Zealand for healthy weight-management6 correctly includes advice to limit consumption of high-sugar foods. However, these guidelines include advice for children and young people to derive most of their energy from grain-based foods and to increase the frequency of consumption of these foods as children move into adolescence. In addition, recommendations to consume dairy products involve promotion of low-fat options, despite evidence that consumption of full-fat dairy products is associated with benefits for both oral health,7 and in weight status and markers of cardiometabolic health in children and adolescents.8 Policy in New Zealand for dental health is focused on prevention of caries in young children with a substantial emphasis on oral hygiene promotion, and recommendations for the consumption of a diet that broadly follows MOH guidelines.
We contend that such recommendations do not reflect the best available evidence for both healthy weight management and maintenance of optimal oral health. Given dental caries is the most common chronic childhood disease in New Zealand, it is imperative that recommendations for healthy eating for New Zealanders reflect the evidence around diet and nutrition for the prevention of dental caries alongside that for other conditions. The consideration of the hormonal theory of metabolic health may resolve the apparent contradictions between the evidence of dietary causes of caries and obesity, and advice provided in dietary guidelines. What follows is an appraisal of the evidence and the state of the current dietary guidelines for children and young people relating to three key areas of diet in dental caries and obesity—sugar, sugar and starch, and full-fat dairy products.
Diet and dental caries
Dental caries can be defined as the localised destruction of susceptible dental hard tissues by the acidic by-products from bacterial metabolism of fermentable carbohydrates.9 Carious lesions on teeth form through a complex interaction between acid-producing bacteria and consumption of fermentable sugars and is influenced by a range of host factors including saliva and dental plaque. Reports from the MOH from 2017 indicate that 40.5% of New Zealand children present with dental caries at age five years. Further, the prevalence of caries measured in young adolescents in New Zealand is estimated to be 38.6%.1
The relationship between high dietary intakes of sugar (sucrose) and dental caries is well established. An extensive systematic review of the relationship between sugar intake and dental caries was conducted by Moynihan and Kelly.10 Positive associations between free sugar intake and dental caries were found in 42 out of 50 studies in children, and in all five studies of adults. These links are both epidemiologically and biologically indicated through several lines of evidence, including studies on the action of bacteria that reside in the oral cavity on a range of sugars in the mouth.11 Time-series analyses of country-level datasets show low levels of dental caries prior to the consumption of refined sugar, and within-person observational studies also show the central role of sugar in the aetiology of dental caries.10
Other fermentable carbohydrates, particularly sugar- and starch-containing foods are also associated with an increased risk of dental caries. In the Western diet, processed starches are found in a wide range of foods and constitute a high percentage of total dietary carbohydrate.9 Studies of the human pH response to a range of starches and enamel/dentin demineralisation show that both sugars and starches are associated with cariogenic activity.12 The total time that plaque pH remains below critical levels of 5.5 upon exposure to processed starch- and sugar-containing foods exceeded that of foods containing high levels of sucrose alone. Through this extended retention of starch-derived sugars in plaque, the effects of other simultaneously present sugars may be prolonged; in which event the consumption of starch has a co-cariogenic effect with that of other sugars. The results from prospective cohort studies show that foods with a relatively low level of sugar but a high proportion of starch were associated with increased caries risk,7 and starch has been identified as an effects modifier in the relationship between dental caries and foods with low sugar levels.7
Conversely, results from prospective cohort studies7,13 and systematic reviews indicate that consumption of full-fat dairy products by children and young people is associated with reduced risks of dental caries and obesity. Neutral or inverse associations were observed in a systematic review by Dror and Allen14 between consumption of milk and dairy products in children and adolescents and dental caries incidence, body fatness and hypertension.14 In addition, dairy product intake was associated with benefits for bone mineralisation and blood pressure. A recent systematic review of 43 cross-sectional studies and 31 prospective studies by Dougkas et al8 found that intake of milk and other dairy products are consistently found to be either not associated or inversely associated with obesity and indicators of adiposity in children, and that there is little evidence to support advice to limit consumption of dairy products for children on the grounds that they may promote obesity.8 Another review by Guo et al15 found a neutral or moderate inverse association between dairy consumption and the risk of developing type-2 diabetes.
The main strategy for the prevention of tooth decay adopted worldwide has been to target children, on the assumption that if caries is prevented in this group, the burden of dental disease would be reduced for all. Strategies for oral health promotion in New Zealand include teaching effective oral hygiene practices, facilitating early access to preventative dental services, promoting use of topical fluorides in toothpaste and promoting healthy eating. However, young New Zealanders present with caries, despite the promotion of a range of oral healthcare practices for the prevention of tooth decay, and caries increases through adolescence and adulthood.16 The focus of conventional dental treatment is primarily on the endpoint of disease and remedial work.17 We argue that the current dental delivery system is not effective in achieving health improvements because this approach does not fully consider the primary cause of disease, the impact of diet and dietary behaviours on dental caries, and the common risk factors for dental caries, other oral diseases and obesity.
Dental caries, obesity and common risk factors
There is mixed evidence about the relationship between the prevalence of dental caries and obesity in children and adolescents. On the one hand, studies in young children have shown that early childhood caries are associated with reduced growth and malnutrition due to insufficient consumption of nutrient-rich food to meet the metabolic and growth needs of children less than two years of age.18 On the other hand, there are stronger associations observed between dental caries, and increased adiposity and obesity in older children and adolescents. Several systematic reviews have examined the cross-sectional relationship between dental caries and increased adiposity using anthropometric measures, including body mass index (BMI) and waist-hip ratio.19 Hayden et al20 reported a statistically significant relationship between adolescent obesity and dental caries (effect size 0.104, p=0.049).20 Similarly, in Chen et al,21 sensitivity analysis work showed obese individuals presented with more dental caries than normal-weight children in their primary teeth (WMD 0.52, 95% CI 0.17 to 0.87, p=0.026). Finally, in a recent prospective cohort study by Li et al, longitudinal associations were observed between dental caries and central obesity measured by a waist-hip ratio among adolescents aged 15–18 years.22
An important caveat when evaluating studies of food consumption, dental caries and obesity, is that much of the evidence comes from cross-sectional and prospective cohort studies. Hence, the observed correlations and relationships cannot be regarded as causal and the findings should be interpreted with some caution.
There is emerging evidence that the ‘calories in, calories out’ model of healthy weight management is too simplistic and ignores the complex nutritional, metabolic and hormonal effects of food. The complex hormonal, neural and microbial feedback systems are likely to be critical in the regulation of satiety, energy partitioning and consequently, body composition. Very young children with decayed teeth may not achieve satiety from meals comprised of a high proportion of nutrient-poor, processed foods, which in turn could then lead to between-meal snacking,23 and abnormally high levels of insulin secretion.5 High levels of insulin production are also associated with the disruption of the satiety hormone leptin, which regulates energy balance and inhibits hunger by signalling to the brain when satiety is achieved from food consumption.5 The consequence of the disruption to leptin promotes a cycle in which hunger and food consumption increases, leading to weight gain.5 Another point is that the frequent consumption of refined snacks comprising sugar and starches is also associated with food addiction characterised by similar behavioural, neurochemical and brain activation responses similar to those of substance abuse.24
Treatments for obesity include dietary interventions, medication, advice to engage in physical exercise, and for morbid obesity: bariatric surgery. There is general agreement within the scientific literature that effective interventions for obesity should comprise dietary interventions to improve metabolic health and achieve weight loss through the consumption of nutrient-rich whole foods,25 long acknowledged to be associated with benefits for dental health and longevity in studies of dietary lifestyles both evolutionarily and modern.26
The predominant dietary prescription in weight loss trials and considered as “best practice” by the MOH is a diet based on a moderate-to-high carbohydrate, moderate protein and low fat intake, with a specific restriction on saturated fat, in the context of an energy deficit.27 However, there is compelling evidence from randomised controlled trials that a restricted carbohydrate intake improves adiposity, glucose metabolism and lipid markers over and above that of the mainstream guidance system.28 These results suggest that a carbohydrate-restriction model should feature prominently in the guidance strategy for promoting health and managing health conditions, and perhaps even be considered the first-line approach in the management of obesity. This approach typically includes less frequent eating, which may impart a dual benefit for caries prevention.
Dietary advice in New Zealand, and contradictions with scientific evidence
New Zealand dietary recommendations for both optimal oral health and weight management usually include advice to adhere to mainstream food and nutrition guidelines. “The Food and Nutrition Guidelines for Healthy Children and Young People (Aged 2–18 years)” are derived from a background paper produced with the purpose of providing background information for health practitioners who provide nutrition advice and develop nutrition programmes.6 These guidelines, endorsed by the MOH, also provide the basis for developing health education resources that are for use by the general public and focus on this age group.
A significant feature of these guidelines is advice to prepare foods or choose pre-prepared foods that are low in sugar, especially added, and to limit the intake of drinks such as cordials, fizzy drinks (including diet drinks and sports drinks) and refined clear fruit juices. The authors of the guidelines recognise that foods high in sugar generally provide very few vitamins and minerals relative to their energy content and that limiting consumption of these foods can be difficult because they are widely available, often inexpensive and heavily marketed to children and young people. The guideline authors also correctly acknowledged the displacement of healthier foods from the diet, given that these foods and drinks contribute to 20% of total energy intake.
However, features of these recommendations are the inclusion of cereals and other processed carbohydrates including breads and baked goods, and strong encouragement to consume low-fat dairy products wherever possible. Additional advice is provided for increasing the frequency of consumption of carbohydrate-containing foods for young people. The advice offered in these guidelines supports high and frequent consumption of carbohydrates. This means that promoted foods include processed items such as breads and cereals, as defined by the NOVA classification system which classifies foods in relation to their degree of processing.29 Further, included in the MOH food suggestions are refined carbohydrates (such as cornflakes) and foods listed in the highest NOVA category of ultra-processed foods, such as plain sweet biscuits and tortillas. This advice for children contradicts evidence of the dietary causes of dental caries and contradicts the nutritional, metabolic and hormonal theory of metabolic health as the cause of obesity. Consumption of breads, cereals and other ultra-processed refined sugar- and starch-containing foods are associated with dental caries,7 is implicated in insulin resistance5 and is associated with obesity in older children and adolescents.20
Since the introduction of dietary guidelines to reduce fat consumption, data from a range of reviews suggests the replacement of saturated fat with sugars and starches are correlated with worldwide obesity and diabetes epidemics.30 Recommendations to consume low-fat dairy products were based on the hypothesis that saturated fats were the primary dietary cause of cardiovascular disease. Although the anti-cariogenic properties of milk products are acknowledged in the guidelines, recommendations about dairy intake promote low-fat dairy products, in direct opposition to epidemiological evidence. Full-fat dairy products have not been associated with obesity in child and adolescent populations, and studies indicate that whole milk consumption is associated with favourable effects on body composition and lipid profiles of children.8,14 In Table 1, specific recommendations provided in the guidelines that relate to healthy eating for weight management and prevention of dental caries are summarised.
Table 1: Specific food and nutrition guidelines for healthy eating in children and young people pertaining to dietary factors and evidence for prevention of obesity and dental caries in young people.
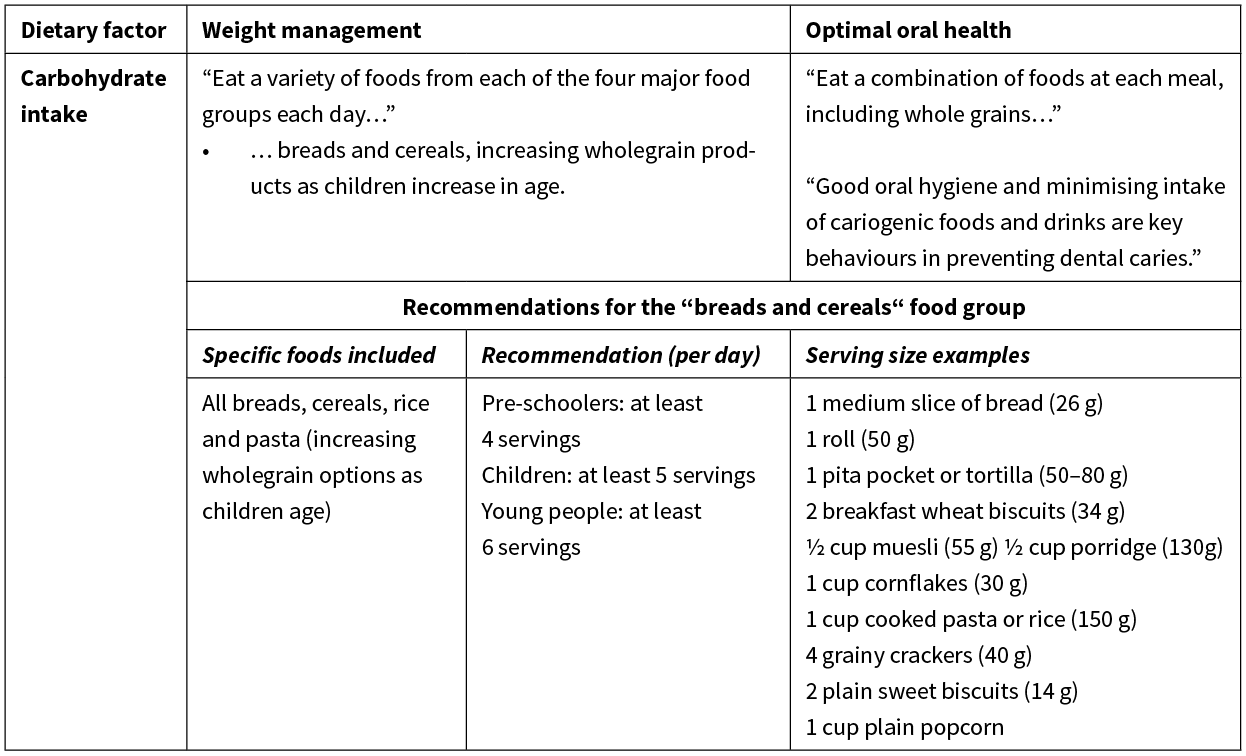
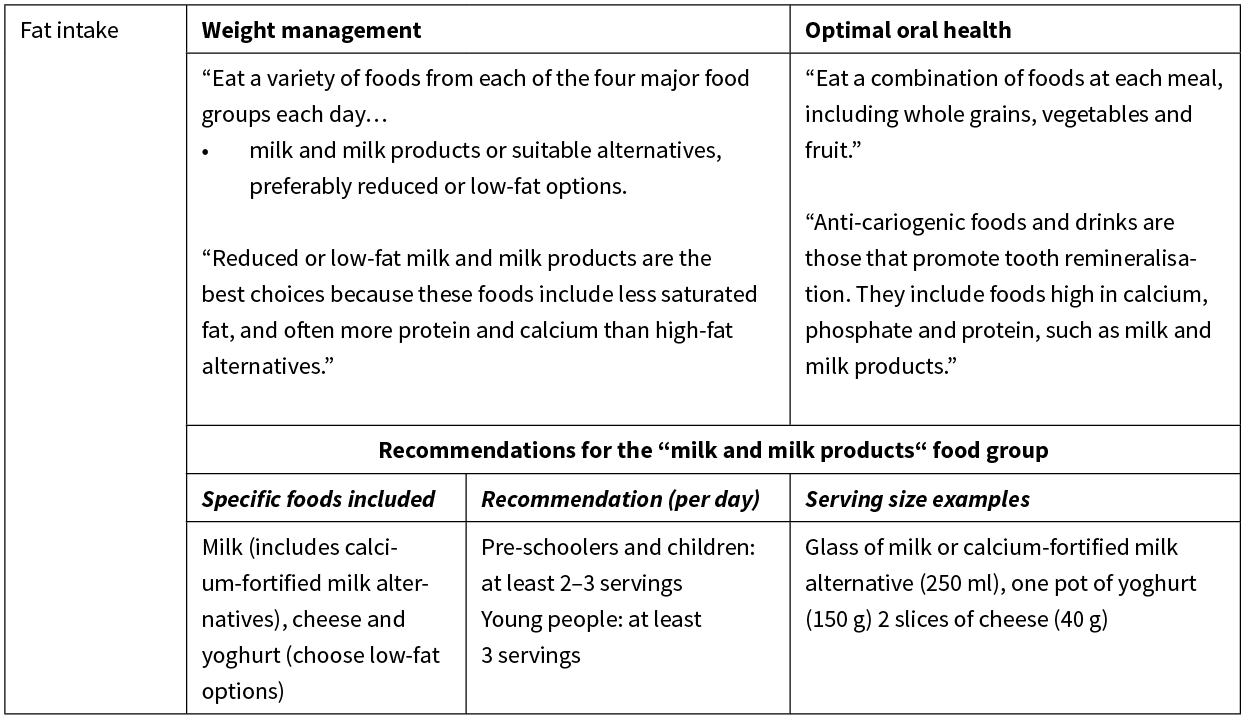
Table 2: Specific food and nutrition guidelines for healthy eating in children and young people relating to meal patterns and evidence for prevention of obesity and dental caries in young people.
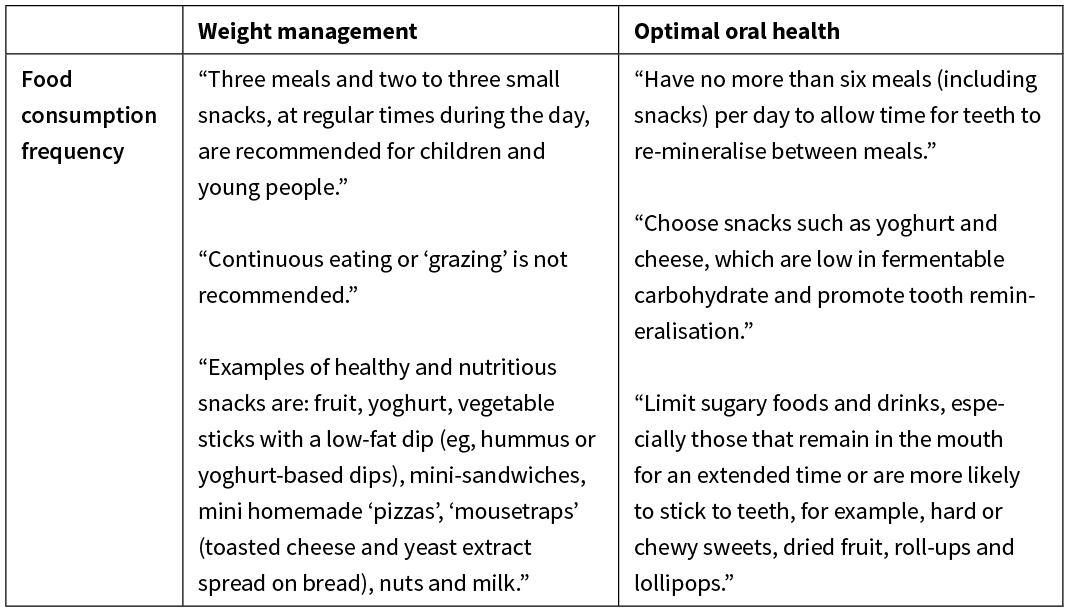
Part 2 of “The Food and Nutrition Guidelines for Healthy Children and Young People (Aged 2–18 years)”6 outlines recommendations for meal patterns of New Zealand children and young people. Three meals plus 2–3 small snacks are recommended during the day at regular times for children and young people. Examples of healthy and nutritious snacks are, according to the guideline: fruit, yoghurt, vegetable sticks with a low-fat dip (eg, hummus or yoghurt-based dips), mini homemade ‘pizzas’, ‘mousetraps’ (toasted cheese and yeast extract spread on bread), nuts and milk. Frequent consumption of carbohydrate-containing foods is also associated with increases in insulin production, down-regulation of leptin hormone action and consequent metabolic dysregulation that promotes an increase in appetite and an alteration of weight homeostasis towards weight gain.17
The recommendation to consume food at a frequency of up to six eating occasions daily contradicts a well-established body of evidence showing a strong relationship between a high-frequency food consumption, and dental caries and the onset of obesity in young people. The inclusion of mini sandwiches and mini homemade “pizzas” as recommended snack foods is also questionable given the high carbohydrate load of these foods. This advice is not informed by evidence that shows clear relationships between the frequent intake of fermentable carbohydrates and the increased risk of dental caries, and other disorders attributable to a high carbohydrate diet. On the contrary, we could find no direct evidence to support both increased consumption of wholegrain products as children age, and to eat from four food groups as stipulated in the guidelines outlined in Table 1. We could not find evidence to support the recommended daily consumption of four, five and six servings per day of breads and cereals of breads for pre-schoolers, children and young people, respectively. In addition, given the anti-cariogenic properties of milk and other full-fat dairy products above, the advice to consume carbohydrate-containing foods as snacks rather than dairy-based food items is likely to be counterproductive.
Conclusions
In conclusion, we have presented evidence that the consumption of foods containing sugar and starches is the principal aetiological factor in dental caries. Intake of these foods are implicated in the increased prevalence of both malnutrition and obesity in children and young people. However, the guidelines for “healthy eating” for children and young people have been produced without consideration of the entirety of evidence relating to the role of not only sugars but also starches, in the aetiology of dental caries and obesity. Furthermore, the evidence relating to reductions in dental caries and adiposity, and markers of cardiometabolic health in children with higher intakes of full-fat dairy products is not reflected in national guidelines. Not only do the dietary guidelines not incorporate the available evidence on healthy eating to prevent dental caries and obesity in young New Zealanders, much of the advice contradicts epidemiological evidence relating to risk factors for dental caries and obesity. Given that the epidemics of dental caries and obesity are a significant and ongoing public health challenge in New Zealand, it is imperative that the guidelines for healthy eating for young New Zealanders incorporate the best dietary advice to improve their health. It is time to update the guidelines and include a dental focus to limit sugar and starch intake and encourage intake of full-fat dairy products to prevent the epidemics of dental caries and obesity, which share a common cause.
Authors
Sarah Hancock, The Human Potential Centre, Auckland University of Technology, Auckland; Caryn Zinn, The Human Potential Centre, Auckland University of Technology, Auckland; Grant Schofield, The Human Potential Centre, Auckland University of Technology, Auckland; Simon Thornley, Section of Epidemiology and Biostatistics, School of Population Health, The University of Auckland, Auckland.Correspondence
Sarah Hancock, The Human Potential Centre, Auckland University of Technology, Auckland.Correspondence email
sarah.hancock@aut.ac.nzCompeting interests
Dr Zinn and Professor Schofield are co-authors of a book series titled “What The Fat”, which assumes a low carbohydrate, healthy fat nutrition approach.1. Ministry of Health, Annual update of key results 2017/18 New Zealand Health Survey. 2019, Ministry of Health: Wellington.
2. Beaglehole R. Sugar sweetened beverages, obesity, diabetes and oral health: a preventable crisis. Pac Health Dialog. 2014; 20(1):39–42.
3. Clarke M, Locker D, Berall G, et al. Malnourishment in a population of young children with severe early childhood caries. Pediatr Dent. 2006; 28(3):254–9.
4. Chi DL, Luu M, Chu F. A scoping review of epidemiologic risk factors for pediatric obesity: Implications for future childhood obesity and dental caries prevention research. J Public Health Dent. 2017; 77 Suppl 1:S8–S31.
5. Weiss R, Bremer AA, Lustig RH. What is metabolic syndrome, and why are children getting it? Ann N Y Acad Sci. 2013; 1281:123–40.
6. Ministry of Health, NZ, Food and Nutrition Guidelines for Healthy Children and Young People (Aged 2–18 years): A background paper. Ministry of Health. 2012, Partial revision February 2015.
7. Campain AC, Morgan MV, Evans RW, et al. Sugar-starch combinations in food and the relationship to dental caries in low-risk adolescents. Eur J Oral Sci. 2003; 111(4):316–25.
8. Dougkas A, Barr S, Reddy S, et al. A critical review of the role of milk and other dairy products in the development of obesity in children and adolescents. Nutr Res Rev. 2019; 32(1):106–127.
9. Selwitz RH, Ismail AI, Pitts NB. Dental caries. Lancet. 2007; 369(9555):51–9.
10. Moynihan PJ, Kelly SA. Effect on caries of restricting sugars intake: systematic review to inform WHO guidelines. J Dent Res. 2014; 93(1):8–18.
11. Loesche WJ, Rowan J, Straffon LH, et al. Association of Streptococcus mutants with human dental decay. Infect Immun. 1975; 11(6):1252–60.
12. Kashket S, Zhang J, Van Houte J. Accumulation of fermentable sugars and metabolic acids in food particles that become entrapped on the dentition. J Dent Res. 1996; 75(11):1885–91.
13. Chankanka O, Marshall TA, Levy SM, et al. Mixed dentition cavitated caries incidence and dietary intake frequencies. Pediatr Dent. 2011; 33(3):233–40.
14. Dror DK, Allen LH. Dairy product intake in children and adolescents in developed countries: trends, nutritional contribution, and a review of association with health outcomes. Nutr Rev. 2014; 72(2):68–81.
15. Guo J, Givens DI, Astrup A, et al. The Impact of Dairy Products in the Development of Type 2 Diabetes: Where Does the Evidence Stand in 2019? Adv Nutr. 2019; Epub ahead of Print: (nmz050, http://doi.org/10.1093 advances nmz050).
16. Broadbent JM, Thomson WM, Poulton R. Trajectory patterns of dental caries experience in the permanent dentition to the fourth decade of life. J Dent Res. 2008; 87(1):69–72.
17. Jatrana S, Crampton P, Filoch, S. The case for integrating oral health into primary health care. The New Zealand Medical Journal. 2009; 122(1301):43–52.
18. Sheiham A. Dental caries affects body weight, growth and quality of life in pre-school children. Br Dent J. 2006; 201(10):625–6.
19. Aas JA, Griffen AL, Dardis SR, et al. Bacteria of dental caries in primary and permanent teeth in children and young adults. J Clin Microbiol. 2008; 46(4):1407–17.
20. Hayden C, Bowler JO, Chambers S, et al. Obesity and dental caries in children: a systematic review and meta-analysis. Community Dent Oral Epidemiol. 2013; 41(4):289–308.
21. Chen D, Zhi Q, Zhou Y, Tao Y, et al. Association between Dental Caries and BMI in Children: A Systematic Review and Meta-Analysis. Caries Res. 2018; 52(3):230–245.
22. Li LW, Wong HM, McGrath CP. Longitudinal Association between Obesity and Dental Caries in Adolescents. J Pediatr. 2017; 189:149–154.
23. Drummond BK, Meldrum AM, Boyd D. Influence of dental care on children’s oral health and wellbeing. Br Dent J. 2013. 11): E27. doi:10.1038/sj.bdj.2013.533
24. Lennerz B, Lennerz JK. Food Addiction, High-Glycemic-Index Carbohydrates, and Obesity. Clin Chem. 2018; 64(1):64–71.
25. Troesch B, Biesalski HK, Bos R, et al. Increased Intake of Foods with High Nutrient Density Can Help to Break the Intergenerational Cycle of Malnutrition and Obesity. Nutrients. 2015; 7(7):6016–37.
26. Woelber JP, Bremer K, Vach K, Konig D, et al. An oral health optimized diet can reduce gingival and periodontal inflammation in humans - a randomized controlled pilot study. BMC Oral Health. 2016; 17(1):28–35.
27. Ministry of Health, New Zealand. Clinical Guidelines for Weight Management in New Zealand Children and Young People. 2016. Wellington, New Zealand.
28. Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition. 2015; 31(1):1–13.
29. Monteiro CA, Cannon G, Levy RB, et al. Ultra-processed foods: what they are and how to identify them. Public Health Nutr. 2019; 22(5):936–941.
30. Harcombe Z. Dietary fat guidelines have no evidence base: where next for public health nutritional advice? Br J Sports Med. 2017; 51(10):769–774.
