CLINICAL CORRESPONDENCE
Vol. 133 No. 1509 |
Osteomyelitis following an undisplaced basal skull fracture
Central skull base osteomyelitis is usually associated with malignant otitis externa or iatrogenic trauma, although cases without these precipitants have been described in at-risk patients (ie, diabetic, immunocompromised).
Full article available to subscribers
Central skull base osteomyelitis is usually associated with malignant otitis externa or iatrogenic trauma, although cases without these precipitants have been described in at-risk patients (ie, diabetic, immunocompromised).1–3 We are not aware of any reported cases of central skull base osteomyelitis following an undisplaced fracture of the temporal bone.
Case report
A 71-year-old male presented with an undisplaced fracture of the right squamo-mastoid portion of the temporal bone on CT scan, following an accidental fall. He is on insulin for type 2 diabetes. On clinical examination, he had a GCS 15/15 and a right haemotympanum. He was observed in a neurosurgical tertiary unit and was discharged after 10 uneventful days.
He re-presented the next day with a head injury following another fall. Clinically, he had incomplete cranial nerves IV and VII palsy and a right hearing loss with a perforated right tympanic membrane. A repeat CT head and an MRI showed a new acute subdural haemorrhage and extension of the basal skull fractures to the sphenoid sinus and pterygoid plate.
He was discharged with a low-grade right earache and non-specific headache. His right ear drum healed within weeks, with ongoing middle ear effusion. Neurologist and maxillofacial surgical opinion found no specific cause of his pains.
Eight months later he presented with gradual worsening of his headaches and fevers; he was treated empirically with systemic antibiotics for suspicion of meningitis. The treatment was discontinued when the lumbar puncture results were negative.
A month later he was readmitted with progressive worsening and severe headaches with raised inflammatory markers (CRP 107, WBC 14.0, Neut 11.8). He had bilateral ear effusions but no abnormality of the ear canals. An MRI brain and high-resolution contrast-CT head showed inflammation and destruction of the right central skull base with an associated soft tissue swelling and sigmoid sinus thrombosis, consistent with central skull base osteomyelitis. He was started on an eight-week course of IV metronidazole and cefepime. His headaches and inflammatory markers improved dramatically.
Discussion
Central skull base osteomyelitis is usually associated with malignant otitis externa or a complication of an invasive procedure. Cases without these precipitants have been reported, with the source of infection hypothesised as arising from the sinuses or blood.3 Patients often have systemic risk factors,3 two of which were present in this case: diabetes and old age.
The most common symptom of skull base osteomyelitis is non-specific headache, which can delay diagnosis, as in this case. Additional symptoms arise from complications; including cranial neuropathies, thrombosis and meningitis, which often occur late in the disease course.2 In many cases inflammatory markers are normal;2 however, raised markers in our patient increased the suspicion of an occult infection.
Often blood cultures are negative and the pathogen is not identified. Previous cases associated with malignant otitis externa have often found Pseudomonas aeruginosa and gram-positive bacteria to be the common pathogens.1,2
CT imaging is generally regarded as a poor diagnostic modality for skull base osteomyelitis. MRI is the modality of choice2 and helped to clinch the diagnosis in this case (Figure 1). Scans that are helpful in monitoring the progress of the treatment include WBC-labelled scans, gallium scintigraphy and PET-CT.
Osteomyelitis is treated aggressively with long-term IV antibiotics, with or without surgical debridement.4 The antibiotic of choice is usually broad spectrum when the organism is not identified.
Figure 1: CT head taken following the patient’s second fall. Right-sided otic sparing undisplaced fracture of the right squamo-mastoid portion of the temporal bone (1), extending to the sphenoid sinus (containing air fluid level) (2).

Figure 2: CT head taken nine months after initial presentation. Soft tissue swelling anterior to the clivus (1), bony destruction anterior right sided aspect of clivus (2). Typical appearance of central skull base osteomyelitis.
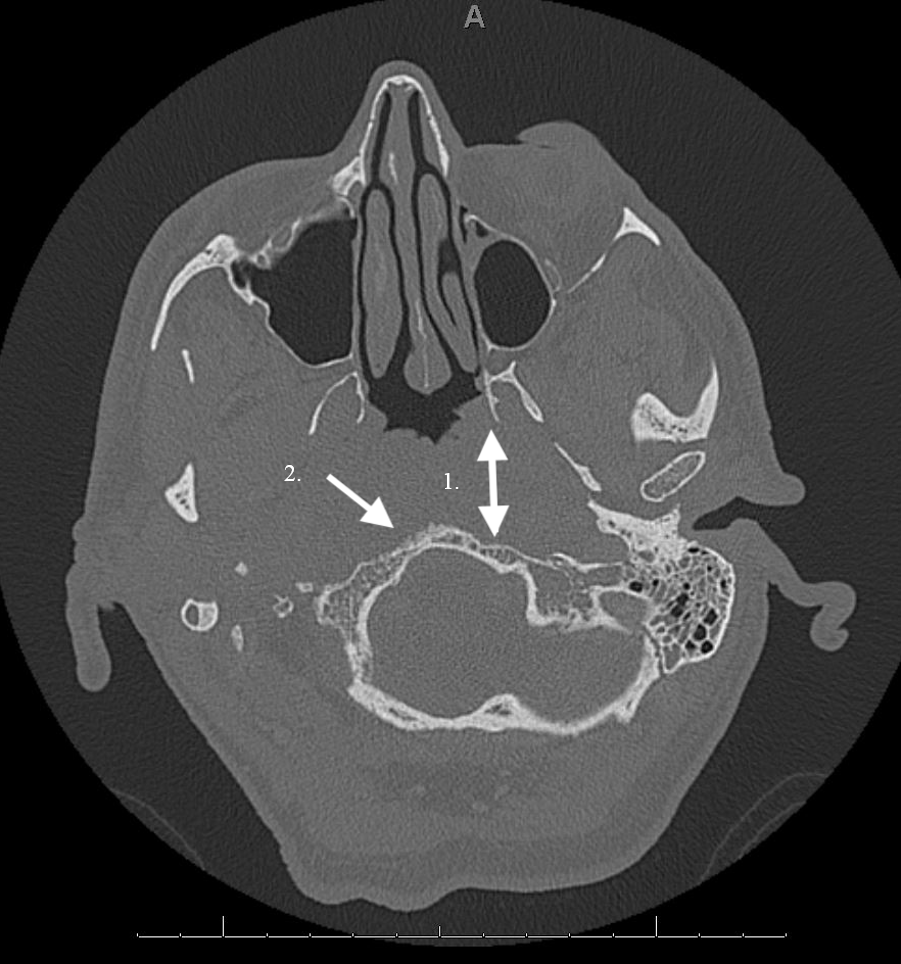
Figure 3: MRI brain (T1) taken nine months after initial presentation. Enhancement of the skull base and anterior soft tissue (1), loss of cortical bone right sided clivus (2), right sigmoid sinus thrombus (3). Typical appearance of central skull base osteomyelitis.

Authors
Kate Seddon, House Officer, Tauranga Hospital, Tauranga; Christopher Low, ENT Consultant, Tauranga Hospital, Tauranga.Acknowledgements
Dr Bruno Carvalho, Consultant Radiologist; Dr Diane Hanfelt-Goade, Consultant Infectious Disease and General Medicine.Correspondence
Dr Kate Seddon, House Officer, Tauranga Hospital, Tauranga.Correspondence email
kate.seddon@bopdhb.govt.nzCompeting interests
Nil.1. Chang, Fishbein, Holliday. Central Skull Base Osteomyelitis in Patients without Otitis Externa: Imaging Findings. American Journal of Neuroradiology, 2003; 24(7):1310–1316.
2. Khan, Quadri, Kazmi, Kwatra, Ramachandran, Gustin, Farooqui, Suriya Zafar. Presentations, a Comprehensive Review of Skull Base Osteomyelitis: Diagnostic and Therapeutic Challenges among Various. Asian Journal of Neurosurgery, 2018; 13(4):959–970.
3. Clark M, Pretorius P, Byren I, Milford C. Central or Atypical Skull Base Osteomyelitis: Diagnosis and Treatment. Skull Base, 2009; 19(4):247–254.
4. Baruah, Kumar, Haque. Acute Osteomyelitis in Closed Fracture of Adult Humerus- Case Report and Review of Literature. IOSR Journal of Dental and Medical Sciences, 2016.
