CLINICAL CORRESPONDENCE
Vol. 133 No. 1510 |
Empyema following laparoscopic appendicectomy—was peritoneal lavage to blame?
A 67-year-old Taiwanese female presented to ED with a history and examination typical of appendicitis.
Full article available to subscribers
A 67-year-old Taiwanese female presented to ED with a history and examination typical of appendicitis. An abdominal CT demonstrated acute uncomplicated appendicitis, and she proceeded to laparoscopic appendicectomy. Intraoperative findings consisted of a swollen appendiceal tip, a friable base but no necrosis or perforation was present. Due to concern regarding a microperforation or microbiological contamination from the friable appendiceal stump, the abdominal cavity was thoroughly washed until returning clear fluid; a total of 2L was used. Histology results later confirmed acute appendicitis and peri-appendicitis.
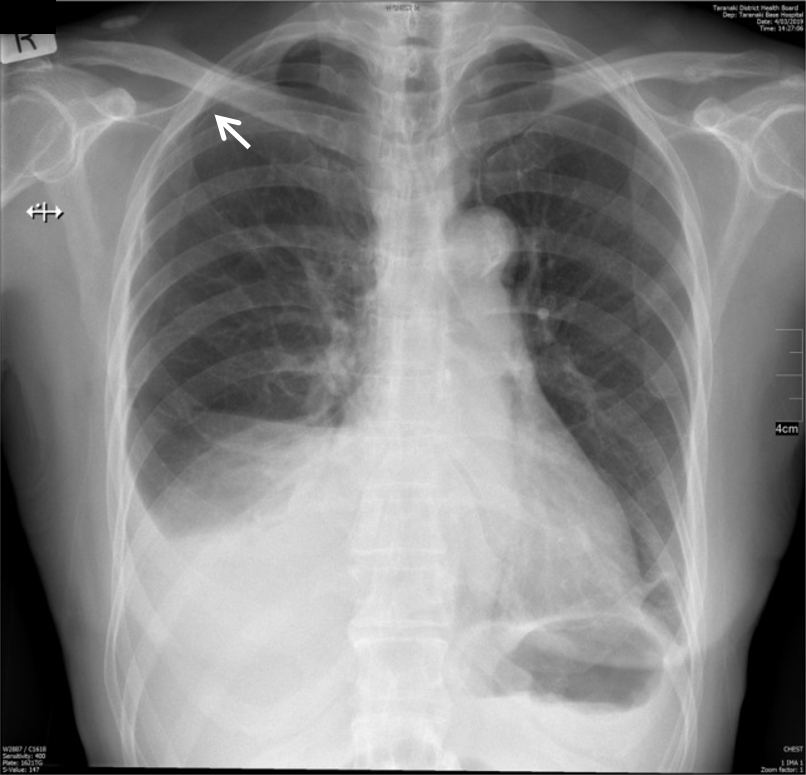
On post-operative day 1, the patient developed right-sided pleuritic chest pain and decreased air entry to the right upper lobe. A CXR indicated a small right pneumothorax and pleural effusion (Figure 1); this was reconfirmed on CT.
Figure 1: Post-operative day 1 chest x-ray showing right-sided pneumothorax and pleural effusion. (Pneumothorax difficult to visualise, indicated by arrow).
IV augmentin was commenced and a diagnostic thoracocentesis performed, draining 400ml of haemoserous fluid. Fluid analysis showed an exudate by Light’s criteria, high WBC (111,729x106/L) and occasional G+ cocci on microscopy. Culture of the fluid grew Escherichia coli; a sample of the aspirate in blood culture bottles also grew Streptococcus anginosus after one day. These findings are consistent with a diagnosis of empyema, with pneumothorax likely arising secondary to this.
Serial CXRs over following days showed worsening of the effusion size and a CRP rise to 280, thus thoracocentesis was repeated on day 6 with <50ml of exudative fluid drained. No organisms were visualised or grown.
On day 6 the patient developed febrile episodes, a rise in the WBC/CRP and recurrence of pleuritic chest pain. Blood cultures were negative. A third thoracocentesis was performed on day 10. Clinically, septations were present and only 100ml of exudative, bloodstained and fibrinous fluid was obtained. A drain was kept in-situ for 72 hours to ensure resolution. Biochemical and clinical improvement was noted with cessation of fevers, normalisation of WBC and down-trending of CRP.
On day 13 the patient was discharged home on oral augmentin but subsequently represented with fevers. Empyema was re-demonstrated on CXR and chest CT but WBC remained normal, CRP low (54) and blood cultures negative. Thus, a conservative approach of IV augmentin was adopted. The patient remained clinically well with down-trending inflammatory markers and was finally discharged on post-operative day 17.
Discussion
Laparoscopic appendicectomy is usually a straightforward operation. Common complications are bleeding, wound infection or abscess formation.1 Empyema is much rarer, with few published case reports.2–4 We believe this is the first documented case of empyema post-laparoscopic appendicectomy in the absence of either perforation or subphrenic abscess.
We believe a congenital right-sided diaphragmatic defect was present, which allowed passage of intra-abdominal wash fluid into the pleural space. Contributory factors included microbiological contamination of the wash fluid from appendix amputation and the patient’s head-down positioning.
No patent diaphragmatic foramina or subphrenic abscesses were visualised on CT, although foramina could not be definitively ruled out without thoracoscopy. The mechanism of the pneumothorax was presumably secondary to empyema, with mainstays of treatment being thoracocentesis/drainage and antibiotics.
At present, many surgeons utilise peritoneal lavage with discretion, the rationale being “the solution to pollution is dilution”. However, there has been a lack of conclusive evidence regarding its efficacy. Most recently, two meta-analyses from 20185 and 20196 indicate no demonstrable benefit of peritoneal lavage in preventing intra-abdominal abscess, wound infections or reducing length of stay. It is important to note there is significant heterogeneity between results of included studies, thus the quality of the evidence is still only moderate.
Though our case occurred due to a combination of factors (including the likely presence of an unknown pre-existing anatomical abnormality), it should still serve as a reminder that interventions with no proven benefit may be associated with complications. Thus, we suggest that usage of peritoneal lavage be wholly avoided, or at least minimised to cases where significant peritoneal contamination has occurred. Furthermore, technique should minimise contamination of the peritoneal cavity beyond the affected area—usually achieved by using small aliquots of irrigation and appropriate patient positioning.7 Hopefully, future studies will provide a definitive answer regarding whether peritoneal lavage provides any clinical benefit, or if it should firmly relegated to a practice of the past.
Authors
Jasmin King, House Officer, Taranaki Base Hospital, New Plymouth; Glenn Farrant, Consultant General Surgeon, Head of General Surgery, Taranaki Base Hospital, New Plymouth.Correspondence
Jasmin King, Taranaki District Health Board, Private Bag 2016, New Plymouth 4342.Correspondence email
jasmin.king@tdhb.org.nzCompeting interests
Nil.1. Andersson RE. Short-term complications and long-term morbidity of laparoscopic and open appendicectomy in a national cohort. Br J Surg. 2014; 101(9):1135–42.
2. Abdulkareem R, Podbielski FJ. “Feculent Empyema after Laparoscopic Appendectomy.” Am Surg. 2018; 1; 84(4):e150–e152.
3. Dietrich A, Nicolas M, Iniesta J, Smith DE. Empyema and lung abscess as complication of a perforated appendicitis in a pregnant woman. Int J Surg Case Rep. 2012; 3(12):622–4.
4. Wong K, Kumar R. Fever following appendicectomy: think about thoracic empyema. NZ Med J. 2007; 1;120(1255).
5. Hajibandeh S, Hajibandeh S, Kelly A, Shah J, Khan RM, Panda N, Mansour M, Malik S, Dalmia S. Irrigation versus suction alone in laparoscopic appendectomy: is dilution the solution to pollution? A systematic review and meta-analysis. Surgical innovation. 2018 Apr; 25(2):174–82.
6. Gammeri E, Petrinic T, Bond-Smith G, Gordon-Weeks A. Meta-analysis of peritoneal lavage in appendicectomy. BJS open. 2019 Feb; 3(1):24–30.
7. LaPlant MB, Saltzman DA, Rosen JI, Acton RD, Segura BJ, Hess DJ. Standardized irrigation technique reduces intraabdominal abscess after appendectomy. Journal of pediatric surgery. 2019 Apr 1; 54(4):728–32.
