ARTICLE
Vol. 133 No. 1510 |
Is the use of health services by older adults in New Zealand associated with their housing tenure?
Internationally and within New Zealand, research has demonstrated an association between housing tenure and health, with home owners generally in better health than renters.
Full article available to subscribers
Internationally and within New Zealand, research has demonstrated an association between housing tenure and health, with home owners generally in better health than renters.1–8 This could be due to features of the home (eg, quality or security) or neighbourhood (eg, safety) influencing health; or individual characteristics such as socioeconomic status or health may influence housing tenure.9,10 In addition, the relationship between tenure and health varies between countries, reflecting different housing contexts, including the availability, quality and security of rental tenure.11–13
New Zealand has had high rates of home ownership but this has been declining, including among older people.14,15 At the same time, New Zealand, along with many other developed countries, is experiencing population ageing, with the number and proportion of older people projected to increase.16,17 This combination of structural ageing together with a tenure revolution has implications for the future need for and provision of health services for older people.
The New Zealand Healthy Ageing Strategy focuses on supporting people to age well and recognises many older people are healthy.18 However, older age can come with increasing levels of disability, frailty and complex comorbidities, and life expectancy in New Zealand has increased faster than health expectancy.17 Older people are higher users of health services; in New Zealand, over 65-year-olds comprise 15% of the population but account for 42% of health service use, and the proportion of health spending on older people is projected to increase.19 The capitation funding for Primary Health Organisations recognises the higher health needs of older people through higher subsidy rates for those aged 65 and older (along with other health-need related characteristics, such as being Māori, Pasifika or holding a high-use health card) but does not consider tenure.20
A range of factors influence an individual’s use of health services, including: health status, the price of services, incomes, individual preferences, whether they are covered by health insurance and characteristics such as age, gender and ethnicity.21–25 The price users pay for health services is affected by government policies as well as insurance coverage. Even within New Zealand’s public health system, the price of health services varies: emergency department, outpatient and inpatient services in public hospitals are provided free of charge, whereas primary healthcare services have charges depending on the patient’s age, Community Services Card or High Use Health Card status, and the PHO and general practice they are enrolled with. Other services such as adult dental care and optometry are paid for privately, and a proportion of the population also hold supplementary private health insurance (covering user charges in primary healthcare and/or care provided by private hospitals or specialists).26
Our earlier research, using data from New Zealand Health Surveys, has shown a health gradient for older New Zealanders, with owner-occupiers in the best health, followed by private renters, while public renters have the poorest health.27 This paper goes on to consider the implications for patterns of health service use and access to care among older renters compared to owner-occupiers. The poorer health status of renters may mean they are (appropriately) higher users of health services than owner-occupiers but cost or other barriers could negate this.
Methods
The New Zealand Health Surveys (NZHS) are national surveys of the New Zealand population aged 15 and over that are conducted annually.28 The surveys use a complex sampling design, including a step to increase the sample sizes of particular ethnic groups (Māori, Pacific and Asian), but have been weighted to produce a representative sample.28 Data from the core NZHS questionnaire allows comparison across years.28 Data for adults aged 55 and over from the 2013/14, 2014/15 and 2015/16 NZHSs were pooled (totalling 15,626 respondents). Confidentialised, unit record files (CURFs) were provided through Statistics New Zealand. The Victoria University of Wellington Ethics Committee advised ethical review was not required to undertake this analysis.
Demographics and measures of healthcare utilisation were compared across three housing tenures: a) owner-occupiers and those living in homes held in a family trust (initially analysed separately but combined due to the similarity of results), b) private renters living in homes owned by private landlords or trusts, and c) public renters in homes owned by city councils, Housing New Zealand and other state-owned organisations. Data were analysed in three age groups: 55–64, 65–74, 75+ years to see if results were a continuation of earlier life experience or changed in older age.
Survey responses were either numerical, a fixed choice with two categories (eg, yes/no) or a list of predetermined categories. The first type of response is presented as weighted means for each tenure group. Tests of differences in means between a) private renters and public renters and b) private renters and owner-occupiers were done using regression for each age category. Responses to other questions were presented as percentages. Tests for differences in percentages between tenure groups were analysed using logistic regression or generalised logistic regression. The resulting p-values were for differences between the marginal means of each tenure group. (For further detail about methods, see27).
Results
Demographics
Demographic data reported previously27 show 83% of the sample were owner-occupiers/family trust (62% and 21% respectively; referred to as owner-occupiers hereafter), 12% were private renters and 5% were public renters. Tenure proportions were similar across age groups, except for slightly more owner-occupiers in the 65–74 year age group (86%). The oldest age group had a higher proportion of women, particularly for private and public renters (66% and 64%) while the other age groups had fairly even proportions of men and women. New Zealand European/Others made up the highest proportion of owner-occupiers (87%). Public renters had higher proportions of Māori (22%) and Pacific people (17%) compared to private renters and owner-occupiers.
Public, then private, renters were more likely to be living alone. Public renters had the lowest, and owner-occupiers the highest, average personal income with the exception for those aged 75+ where there was no significant difference between private renters and owner-occupiers (14% missing data for this question).
Overall health status—SF-12
The Medical Outcomes Study Short Form version 2.0 (SF-12) is an internationally validated instrument which was used to gain an overall measure of physical and mental health29 (see Figure 1). Both showed a health gradient: public renters in the poorest physical and mental health, followed by private renters, with owner-occupiers in the best overall health. Self-reported physical and mental health conditions, risk factors and health behaviours also showed owner-occupiers generally had the best health and public renters the poorest (for full details of these results, see27).
Figure 1: Average SF-12 Physical Health Score and SF-12 Mental Health Score for owner-occupiers, private renters and public renters aged 55+.
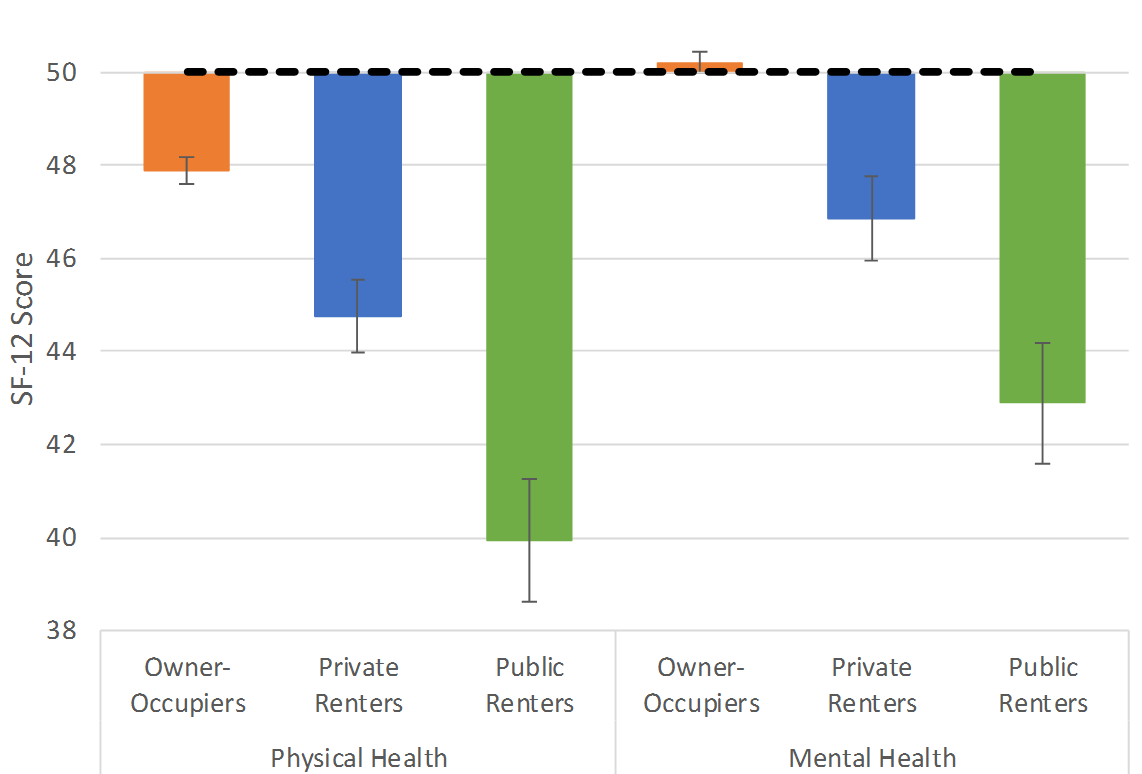
The dashed line represents the population average for each statistic for New Zealanders aged 15+.
Health service utilisation
In the text, we focus on health service utilisation results, which are both statistically and practically significant (p value <0.05 and, where relevant, a five-percentage-point difference between groups). Main results (including confidence intervals) are shown in Tables 1–4.
Primary care
Table 1 shows primary care utilisation. Most respondents said they had a GP clinic or medical centre they usually attend when feeling unwell or injured, with no significant differences between tenure groups. Most older people had seen a GP in the past year. Among 55-64 year olds, public renters were more likely to report seeing a GP and both public and private renters in this age group reported more visits: annual visits averaged 5.5 for public renters, 4.4 for private renters and 3.3 for owner-occupiers.
Table 1: Health service utilisation: primary care.
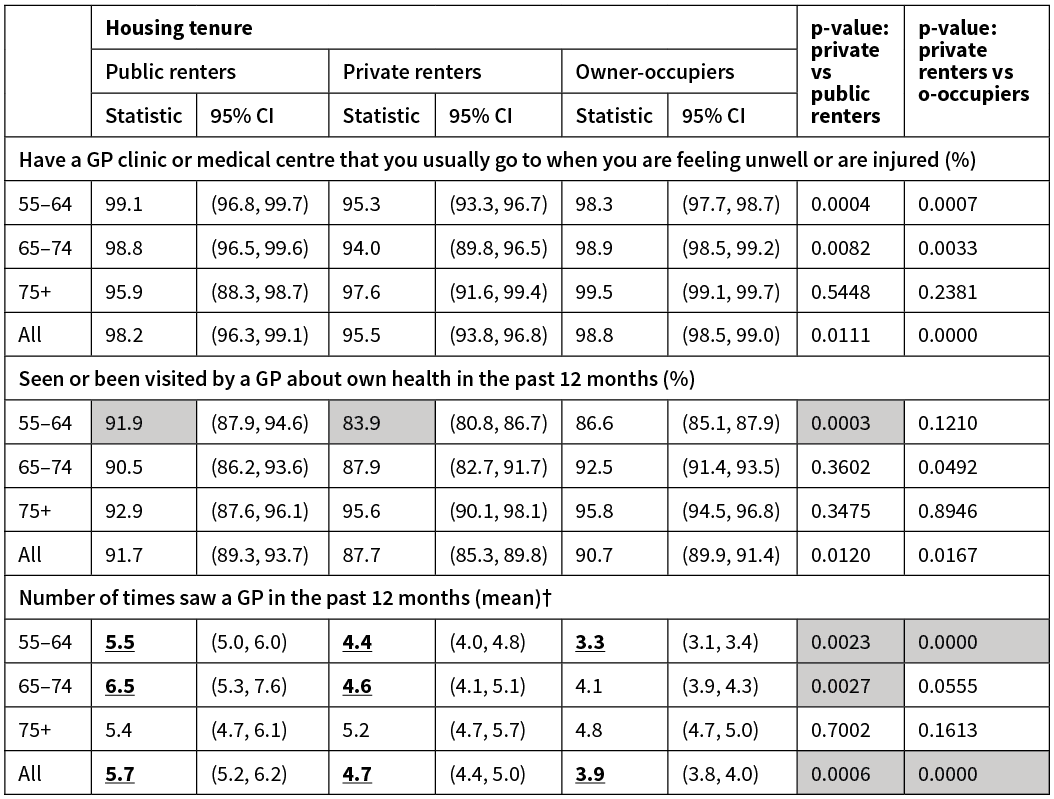
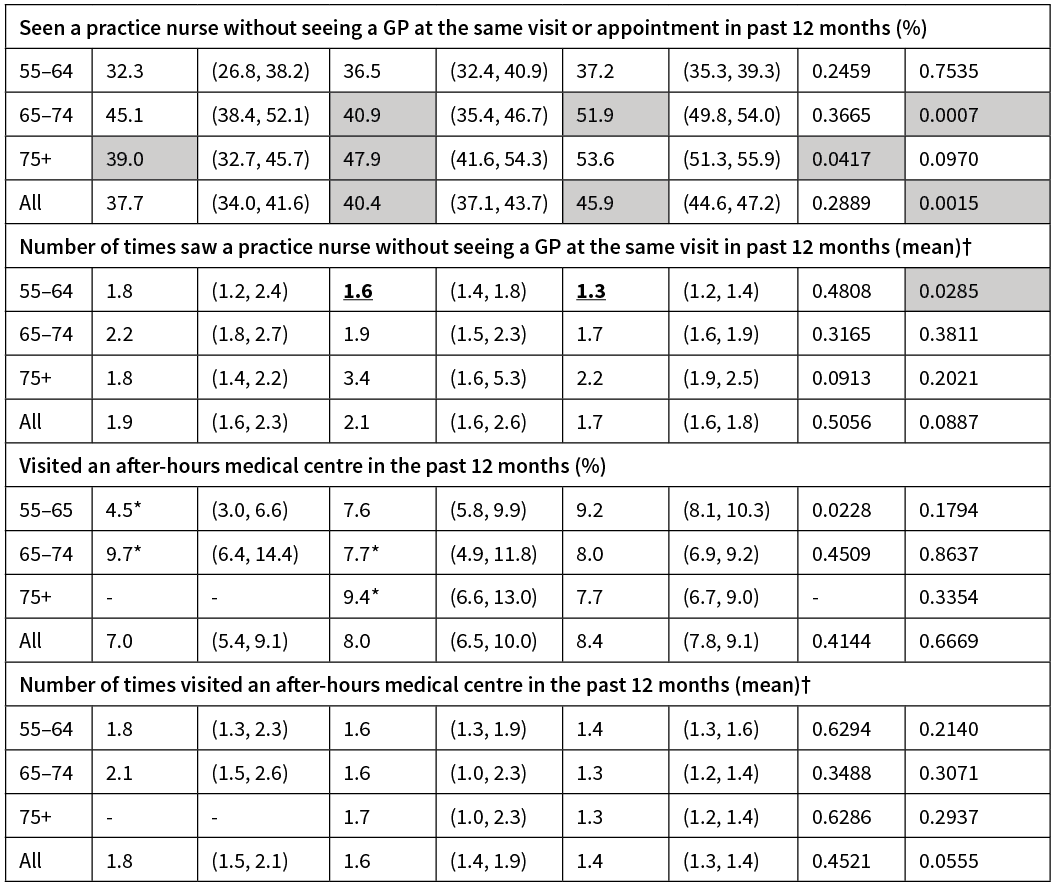
Estimates with a relative sampling error (RSE) of 30–50% are marked with an asterisk (*) and should be used with caution. Any estimates containing fewer than 30 respondents are suppressed (-). Results with shading highlight indicate differences that are both statistically significant (p value <0.05) and likely to be practically significant (five percentage-point difference between groups). Results in bold indicate a statistically significant difference (p value <0.05).†For those who used this service.
Private renters aged 65–74 and public renters aged 75+ were less likely to have seen a practice nurse without seeing a GP at the same visit. The number of visits to a practice nurse alone in the past year was significant only for private renters aged 55–64 (mean 1.6) compared with owner-occupiers (1.3). There were no significant differences in the proportion of respondents who had visited an after-hours medical centre (AHMC) in the past year or the number of visits to an AHMC.
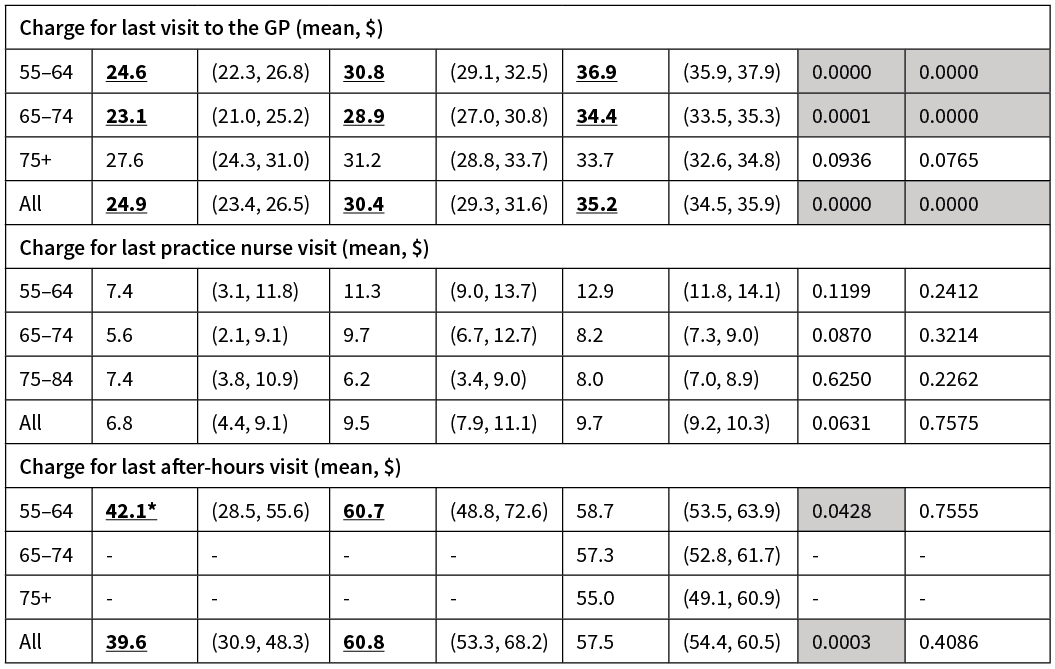
Among the younger two age groups, public then private renters were charged a lower fee for their last GP visit than owner-occupiers. There were no significant differences between average charges to see the practice nurse.
Secondary care
Table 2 shows secondary care service utilisation. Among the 55–64 age group, public then private renters were more likely than owner-occupiers to have used a service at or been admitted to a public hospital (44%, 35% and 27% respectively). Public renters aged 65–74 were also more likely than the other two tenure groups to have used these services.
Table 2: Health service utilisation: secondary care.
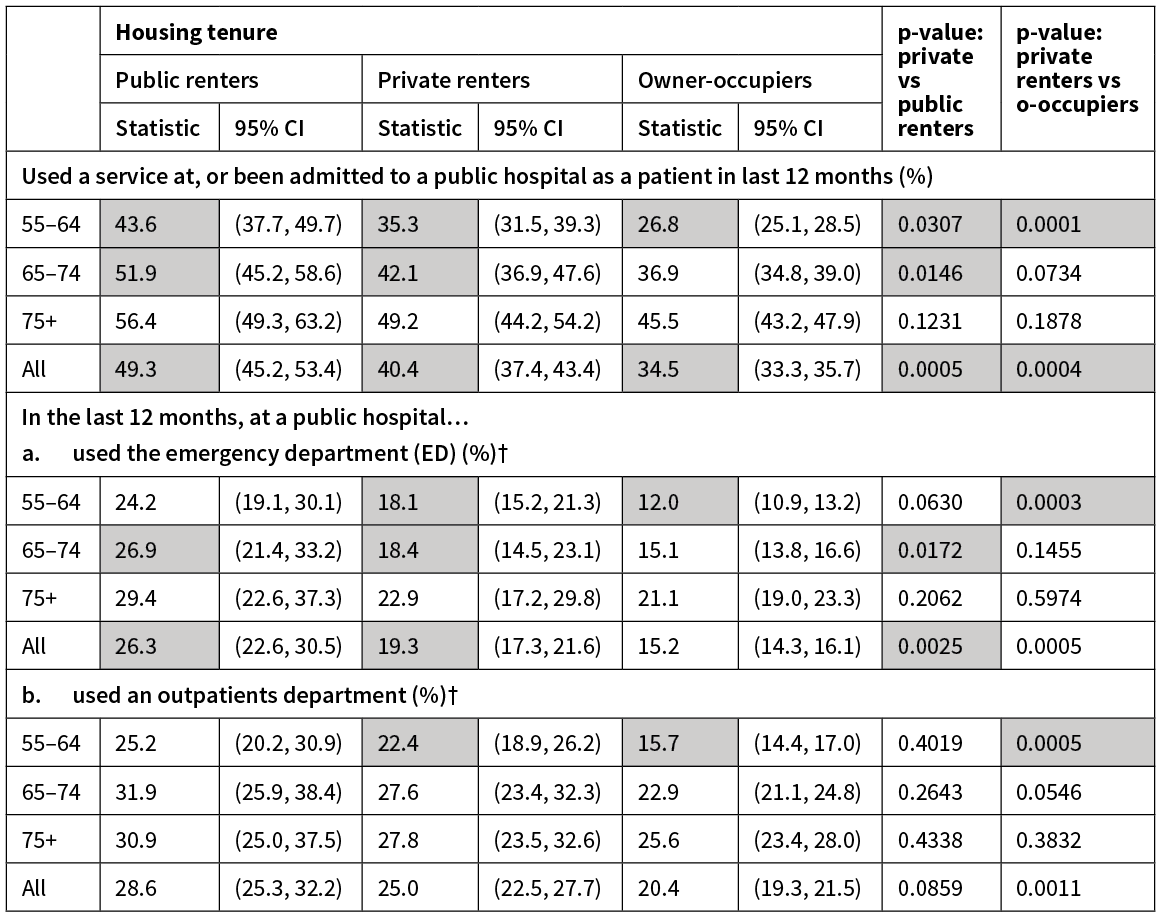
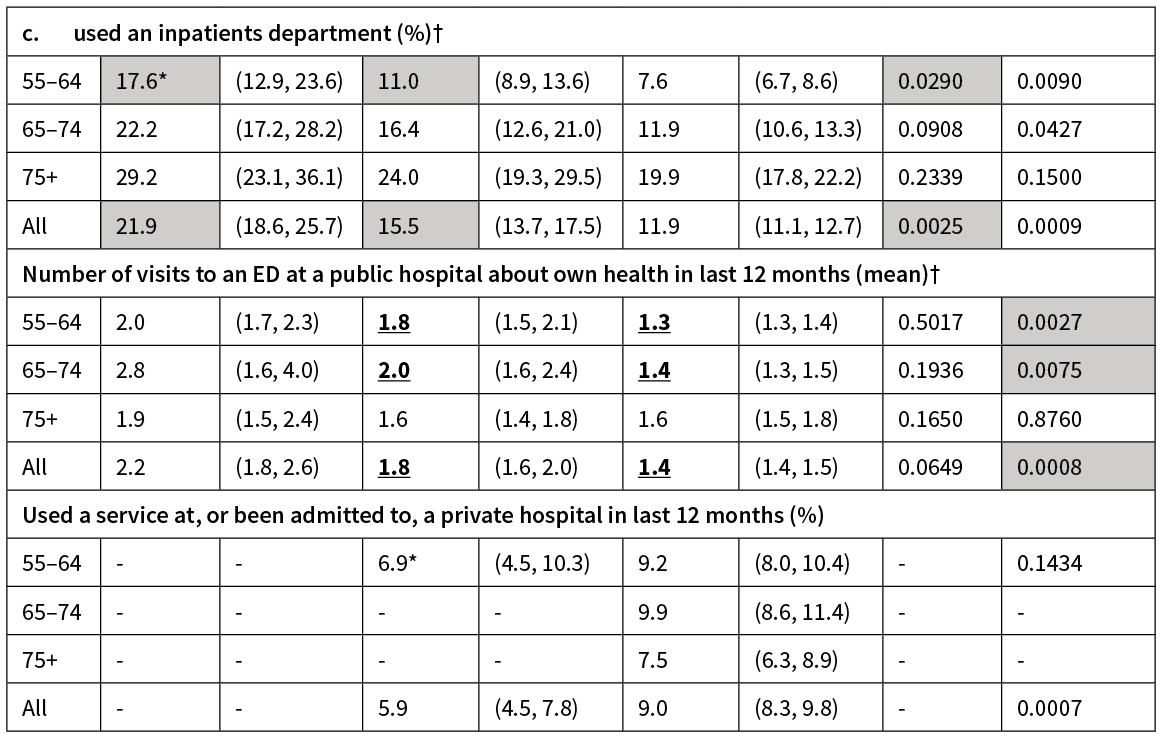
Estimates with an RSE of 30-50% are marked with an asterisk (*) and should be used with caution. Any estimates containing fewer than 30 respondents are suppressed (-). Results with shading highlight indicate differences that are both statistically significant (p value <0.05) and likely to be practically significant (five percentage-point difference between groups). Results in bold indicate a statistically significant difference (p value <0.05).† For those who used this service.
Renters were more likely than owner-occupiers to have used an emergency department (ED) in the last year (significant differences for private renters aged 55–64 and public renters aged 65–74). Owner-occupiers made fewer ED visits in the last 12 months than renters among the two younger age groups.
Among those aged 55–64, public renters were more likely to have used an inpatients department in the last year, and private renters were more likely than owner-occupiers to have used an outpatient department. Fewer than 10% of owner-occupiers had used private hospital services in the last 12 months; the number of renters using these services was too small for analysis.
Dental and other healthcare workers
Overall, renters were less likely than owner-occupiers to have visited a dental healthcare worker in the last year (Table 3). Differences were significant for private renters in the younger two age groups and public renters in the oldest two age groups. Among the two younger age groups, owner-occupiers were more likely to report seeing an optician or optometrist. The number of respondents who visited other health professionals (eg, pharmacist, physiotherapist, chiropractor) or who had seen a listed medical specialist (eg, cardiologist, oncologist, respiratory physician, geriatrician) in the last year was too small to allow for analysis or showed no significant differences.
Table 3: Health service utilisation: dental health care, other healthcare workers.
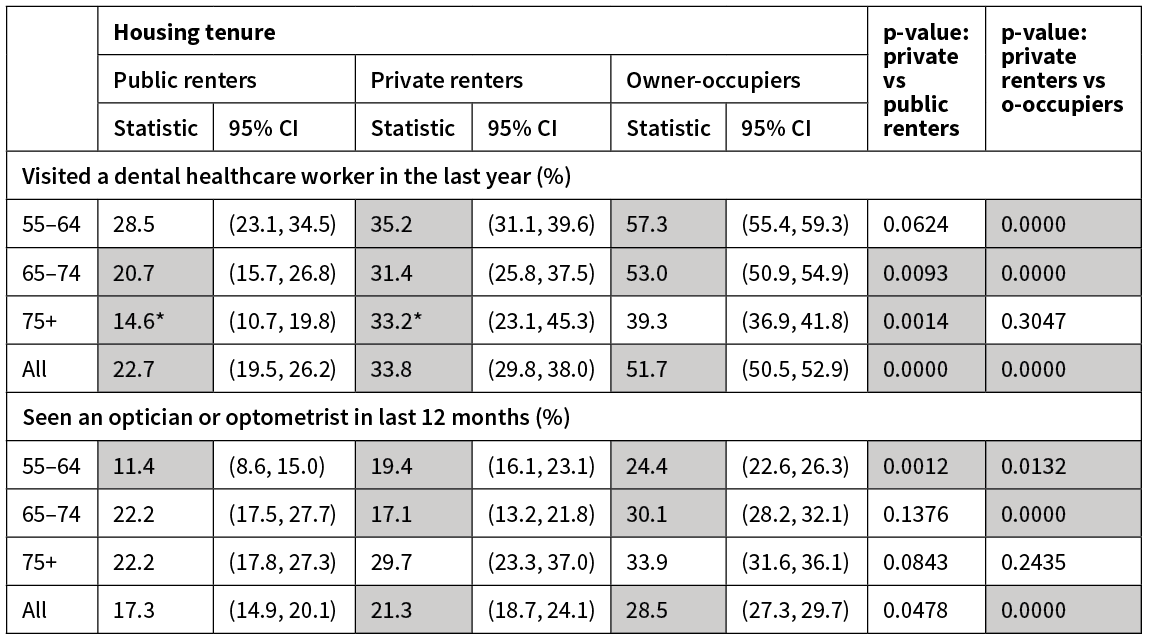
Estimates with an RSE of 30–50% are marked with an asterisk (*) and should be used with caution. Results with shading highlight indicate differences that are both statistically significant (p value <0.05) and likely to be practically significant (five percentage-point difference between groups).
Unmet need
Among 55–64 and 65–74 age groups, renters were more likely to report cost as a barrier to visiting a GP, an AHMC or dental health carer or to picking up one or more prescription items (Table 4).
Table 4: Unmet need.
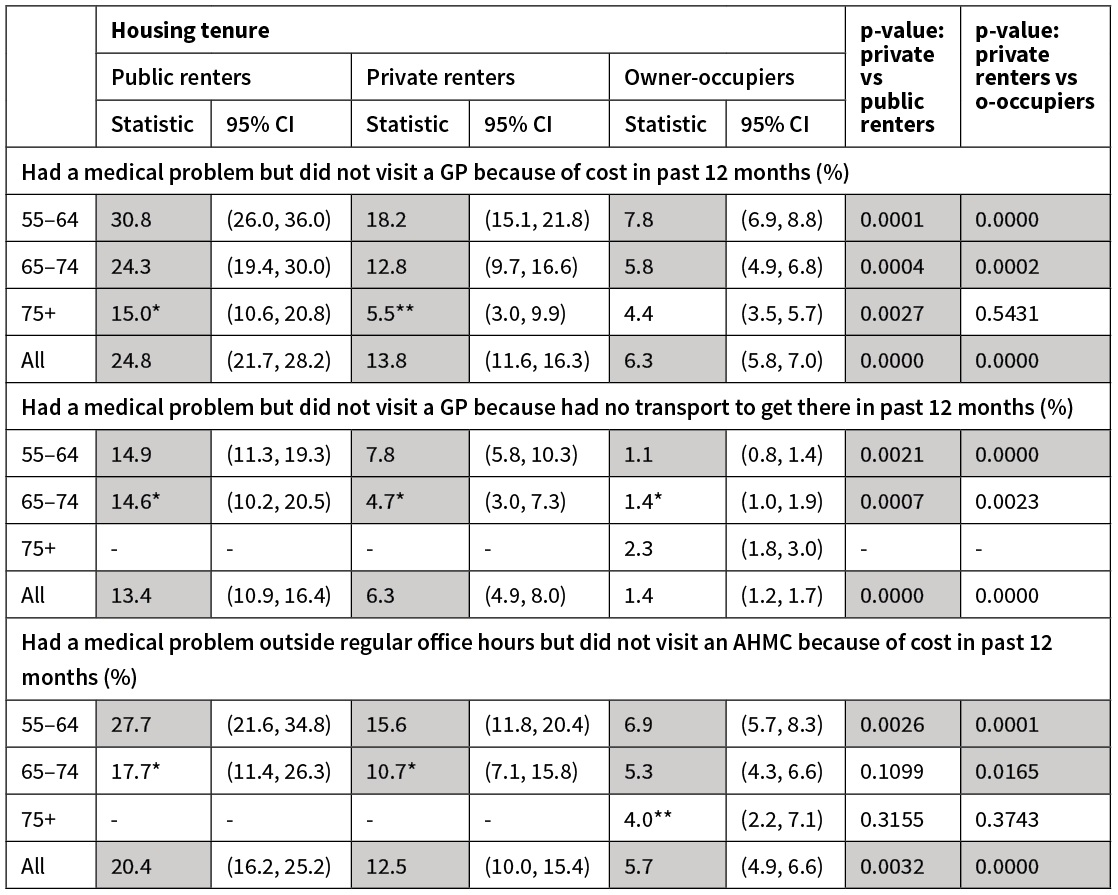
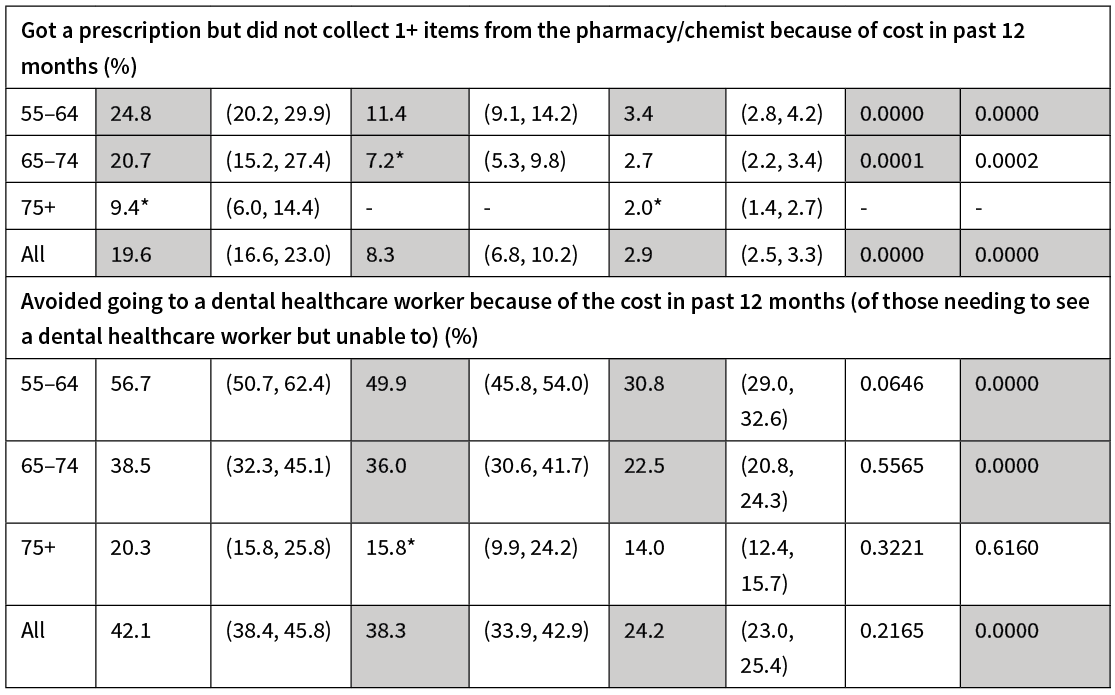
Estimates with an RSE of 30–50% are marked with an asterisk (*) and should be used with caution, those with an RSE over 50% are marked with a double asterisk (**) and should be considered unreliable for most practical purposes, any estimates containing fewer than 30 respondents are suppressed (-). Results with shading highlight indicate differences that are both statistically significant (p value <0.05) and likely to be practically significant (five percentage-point difference between groups).
Public renters in the two younger age groups and private renters aged 55–64 were more likely to report lack of transport had prevented them visiting a GP.
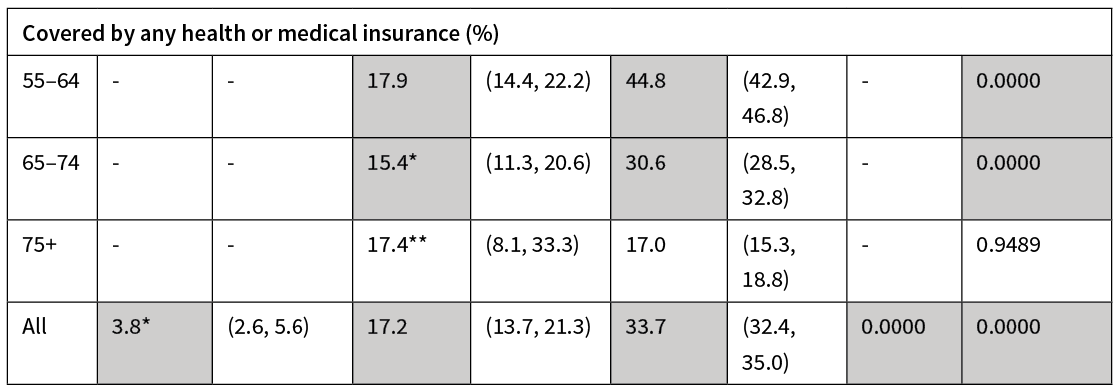
Health insurance coverage
Too few public renters were covered by any health insurance for analysis. Among the 55–64 and 65–74 year olds, owner-occupiers were more likely than private renters to have health insurance (Table 4).
Discussion
In the 55–64 and 65–74 year age groups, renting—particularly publicly—rather than owning was associated with higher use of some public health services, including GP visits, public hospital or ED use in the last year. The same general trend was seen across the majority of variables relating to use of public primary and secondary care services even when not statistically significant. There were very few significant differences between tenure groups among those aged 75 years and over. Our earlier work showed poorer health among renters compared with owner-occupiers,27 so higher health service use may appropriately reflect need.
Renters were generally less likely to report using privately paid services such as dental and optician services, potentially adversely impacting their health.30,31 Very few public renters had health/medical insurance or had used a service at a private hospital in the last year.
While public renters made more visits to the GP in the two younger age groups, they were also charged the lowest co-payment. However, there are indications that high levels of unmet need remain, with renters more likely to report lack of transport or cost impeded a necessary visit to a GP, AHMC or dental health worker or to collecting a prescription item. Poor access to primary care and medications can be associated with poorer outcomes or costly secondary care.32,33
A strength of this paper is that it draws upon a large, nationally representative dataset and adds to the literature on the relationship between tenure and health service use. Limitations include the self-reporting of health service use measures and the cross-sectional nature of the study, which means we are unable to make any conclusions regarding causality. However, tenure provides a marker of potential health need. Determining the mechanisms through which associations between tenure, health and use of health services operate will be important for directing future policy and interventions. These could include addressing features of rental housing that may impact on health (eg, through the provision of suitable rental stock for older people, security of tenure or regulations about insulation34) and ensuring health services address the needs of renters (eg, through supporting housing modifications when needed to enable continuing home care).
Further research exploring the relationship between tenure and use of other health and care services utilised more among older adults—such as home care and aged residential care—would be valuable in building up a broader picture of service use among older public and private renters. Many older people want to continue to live at home, supported by health services as needed,18 and this may also be less costly than residential care services. However, in other countries, older renters have been shown to be more likely to enter residential care.35–40 Aged residential care accounts for around 60% of New Zealand’s district health board expenditure on support services for older people,19 and so any relationship between tenure and transition to residential care will be particularly important in assessing future demand and the budgetary implications associated with a growing proportion of older renters.
New Zealand has a growing number and proportion of older adults, and at the same time, falling home ownership rates. Although the analyses here demonstrate association not causation, if renting does in part lead to increases in service use, rising numbers of older renters living in poorer health than owner-occupiers could mean an increase in demand for some health and care services in future—and additional personal and government expenditure as a result to ensure that the health needs of the population are met. Some groups are particularly vulnerable to these changes, with higher rates of renting among Māori and Pacific people and older females (aged 75+). As older renters were also more likely to be on lower incomes and living alone, policy-makers will need to consider how they can better support older renters through health and social services delivery, housing and income support.
Aim
To explore associations between tenure and the health service use of older New Zealanders.
Methods
Analysis of pooled data for adults aged 55+ from three New Zealand Health Surveys (2013/14, 2014/15, 2015/16) comparing owner-occupiers, private renters and public renters.
Results
Public renters, and in some age groups private renters, reported more visits to the GP and a higher proportion reported using a public hospital service in the last year. Renters were less likely than owner-occupiers to have used some privately paid services (visiting a dental health worker or optician). Renters averaged lower co-payments for their last GP visit, but financial barriers to accessing a GP, after-hours medical centre use and not collecting prescriptions were more likely to be reported by renters than owner-occupiers—particularly those that rent publicly.
Conclusion
New Zealanders are simultaneously living longer while having declining opportunities to enter home ownership. Older renters are more likely to live in poorer health and, overall, are more likely to use some (public) health services than owner-occupiers yet are more likely to have unmet health needs. The increasing reliance on renting among older people has implications for population health and wellbeing, health service delivery and transitions to residential care.
Authors
Megan Pledger, Senior Research Fellow, Health Services Research Centre, Faculty of Health, Victoria University of Wellington, Wellington; Phoebe Dunn, Research Fellow, Health Services Research Centre, Faculty of Health, Victoria University of Wellington, Wellington; Janet McDonald, Senior Research Fellow, Health Services Research Centre, Faculty of Health, Victoria University of Wellington, Wellington; Jacqueline Cumming, Professor of Health Policy and Management, Health Services Research Centre, Faculty of Health, Victoria University of Wellington, Wellington; Kay Saville-Smith, Director, Centre for Research, Evaluation and Social Assessment (CRESA), Wellington.Acknowledgements
We would like to the respondents of the New Zealand Health Survey in 2013/14, 2014/15 and 2015/16 for their participation in the survey, and Ruth Fraser for her administrative support for the research team. This research was part of a four-year programme called ‘Life When Renting’ (see http://renting.goodhomes.co.nz). It was funded through the New Zealand Ageing Well National Science Challenge (www.ageingwellchallenge.co.nz) [contract number 12815/1 SUB 1321].Correspondence
Megan Pledger, Senior Research Fellow, Health Services Research Centre, Faculty of Health, Victoria University of Wellington, PO Box 600, Wellington 6140.Correspondence email
megan.pledger@vuw.ac.nzCompeting interests
Access to the data used in this study was provided by Statistic New Zealand under conditions designed to keep individual information secure in accordance with requirements of the Statistics Act 1975. The opinions presented in this article are those of the authors and do not necessarily represent an official view of Statistics New Zealand.1. Barrett P, Twitchin S, Kletchko S, Ryan F. The living environments of community-dwelling older people who become frail: another look at the Living Standards of Older New Zealanders survey. Social Policy Journal N Z. 2006; (28):133–57.
2. Chandola T. Social class differences in mortality using the new UK National Statistics Socio-Economic Classification. Soc Sci Med. 2000 Mar; 50(5):641–9.
3. Clair A, Hughes A. Housing and health: new evidence using biomarker data. J Epidemiol Community Health. 2019 Mar; 73(3):256–262.
4. Ellaway A, Macdonald L, Kearns A. Are housing tenure and car access still associated with health? A repeat cross-sectional study of UK adults over a 13-year period. BMJ Open. 2016 Nov 2; 6(11):e012268.
5. Jatrana S, Blakely T. Socio-economic inequalities in mortality persist into old age in New Zealand: Study of all 65 years plus, 2001–04. Ageing Soc. 2014; 34(6):911–29.
6. Laaksonen M, Tarkiainen L, Martikainen P. Housing wealth and mortality: A register linkage study of the Finnish population. Soc Sci Med. 2009 Sep; 69(5):754–60.
7. Matthews RJ, Jagger C, Hancock RM. Does socio-economic advantage lead to a longer, healthier old age? Soc Sci Med. 2006; 62(10):2489–99.
8. Pollack CE, von dem Knesebeck O, Siegrist J. Housing and health in Germany. J Epidemiol Community Health. 2004 Mar; 58(3):216–22.
9. Connolly S. Housing tenure and older people. Rev Clin Gerontol. 2012; 22(4):286–92.
10. Shaw M. Housing and public health. Annu Rev Public Health. 2004; 25:397–418.
11. Dalstra JAA, Kunst AE, Mackenbach JP. A comparative appraisal of the relationship of education, income and housing tenure with less than good health among the elderly in Europe. Soc Sci Med. 2006; 62(8):2046–60.
12. Herbers DJ, Mulder CH. Housing and subjective well-being of older adults in Europe. J Hous Built Environ. 2017; 32(3):533–58.
13. Huisman M, Kunst AE, Andersen O, et al. Socioeconomic inequalities in mortality among elderly people in 11 European populations. Journal Epidemiol Community Health. 2004; 58(6):468–75.
14. Jackson N, James B. Home ownership, renting, and residence in a home owned by a family trust for the Western Bay of Plenty and total New Zealand, by birth cohort, for the period 1986-2013. 2016. Available from: http://renting.goodhomes.co.nz/wp-content/uploads/2017/06/wbop-cohort-report-final2.pdf
15. Statistics New Zealand. 2013 Census QuickStats About Housing. 2014. Available from: http://archive.stats.govt.nz/~/media/Statistics/Census/2013%20Census/profile-and-summary-reports/quickstats-about-housing/quickstats-housing.pdf
16. United Nations Department of Economic and Social Affairs, Population Division. World population ageing 2015. New York: UN; 2015.
17. Ministry of Health. Older people’s health: Our changing population. 2016. Available from: http://www.health.govt.nz/nz-health-statistics/health-statistics-and-data-sets/older-peoples-health-data-and-stats/our-changing-population
18. Associate Minister of Health. Healthy ageing strategy. Wellington: Ministry of Health; 2016.
19. Ministry of Health. DHB spending on services for older people. 2016. Available from: http://www.health.govt.nz/nz-health-statistics/health-statistics-and-data-sets/older-peoples-health-data-and-stats/dhb-spending-services-older-people
20. Ministry of Health. Capitation rates. 2019. Available from: https://www.health.govt.nz/our-work/primary-health-care/primary-health-care-subsidies-and-services/capitation-rates
21. Cumming J, Stillman S, Liang Y, et al. The determinants of GP visits in New Zealand. Aust N Z J Public Health. 2010; 34(5):451–7.
22. Jatrana S, Crampton P, Norris P. Ethnic differences in access to prescription medication because of cost in New Zealand. J Epidemiol Community Health. 2011; 65(5):454–60.
23. Scott K, Marwick J, Crampton P. Utilization of general practitioner services in New Zealand and its relationship with income, ethnicity and government subsidy. Health Serv Manage Res. 2003; 16(1):45–55.
24. Crampton P, Jatrana S, Lay-Yee R, Davis P. Exposure to primary medical care in New Zealand: number and duration of general practitioner visits. N Z Med J. 2007; 120(1256):U2582.
25. Jatrana S, Crampton P. Primary health care in New Zealand: who has access? Health policy. 2009; 93(1):1–10.
26. Cumming J, McDonald J, Barr C, et al. New Zealand health system review (Health Syst Transit. 2014; 4(2).
27. Pledger M, McDonald J, Dunn P, et al. The health of older New Zealanders in relation to housing tenure: analysis of pooled data from three consecutive, annual New Zealand Health Surveys. Aust N Z J Public Health. 2019; 43(2):182–189.
28. Ministry of Health. New Zealand Health Survey. 2019. Available from: http://www.health.govt.nz/nz-health-statistics/national-collections-and-surveys/surveys/new-zealand-health-survey
29. Ministry of Health. Content guide 2015/16: New Zealand Health Survey Wellington: Ministry of Health; 2016. Available from: http://www.health.govt.nz/publication/content-guide-2015-16-new-zealand-health-survey
30. Hollister MC, Weintraub JA. The association of oral status with systemic health, quality of life, and economic productivity. J Dent Educ. 1993; 57(12):901–12.
31. Mojon-Azzi SM, Sousa-Poza A, Mojon DS. Impact of low vision on well-being in 10 European countries. Ophthalmologica. 2008; 222(3):205–12.
32. Heisler M, Langa KM, Eby EL, et al. The health effects of restricting prescription medication use because of cost. Med Care. 2004 Jul; 42(7):626–34.
33. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005; 83(3):457–502.
34. Ministry of Business, Innovation & Employment. Tenancy services: Insulation. 2019. Available from: http://www.tenancy.govt.nz/maintenance-and-inspections/insulation/
35. Australian Institute of Health and Welfare. Patterns in use of aged care 2002–03 to 2010–11. Canberra: AIHW; 2014. Available from: http://www.aihw.gov.au/reports/aged-care/patterns-in-use-of-aged-care-2002-03-to-2010-11/contents/table-of-contents
36. Grundy E, Jitlal M. Socio-demographic variations in moves to institutional care 1991–2001: a record linkage study from England and Wales. Age Ageing. 2007; 36(4):424–30.
37. Luppa M, Luck T, Weyerer S, et al. Prediction of institutionalization in the elderly. A systematic review. Age Ageing,. 2009:afp202.
38. Martikainen P, Nihtilä E, Moustgaard H. The effects of socioeconomic status and health on transitions in living arrangements and mortality: a longitudinal analysis of elderly Finnish men and women from 1997 to 2002. J Gerontol B Psychol Sci Soc Sci. 2008; 63(2):S99–S109.
39. McCann M, Grundy E, O’Reilly D. Why is housing tenure associated with a lower risk of admission to a nursing or residential home? Wealth, health and the incentive to keep ‘my home’. J Epidemiol Community Health. 2012; 66(2):166–9.
40. Rouwendal J, Thomese F. Homeownership and Long-Term Care. Hous Stud. 2013; 28(5):746–63.
