CLINICAL CORRESPONDENCE
Vol. 133 No. 1511 |
Hypothyroidism causing bilateral lower-limb compartment syndrome
A 17-year-old Indian man was referred to hospital with bilateral anterior leg pain and difficulty walking after a forty-minute session of recreational basketball 36 hours prior.
Full article available to subscribers
Case report
A 17-year-old Indian man was referred to hospital with bilateral anterior leg pain and difficulty walking after a forty-minute session of recreational basketball 36 hours prior. There was no history of trauma. He took no regular medications. His family history was significant for maternal Grave’s disease and two grandparents having type 2 diabetes mellitus.
Physical examination revealed diffuse erythema and non-pitting oedema over the anterior tibial compartments bilaterally, minimal tenderness on palpation, restricted passive dorsiflexion of the ankles and a high stepping gait with bilateral foot drop. Power was grade 1/5 in the ankle dorsiflexors with paraesthesiae of the dorsum of both feet. Ankle and toe plantarflexion were normal with symmetrical deep tendon reflexes in both lower extremities. Peripheral pulses were intact. His hair, skin and nails were normal. There were no palpable neck masses or thyromegaly. The remainder of the systemic examination was also normal, including cardiorespiratory examination and clinical euvolemia.
Laboratory investigations revealed a CK >22,000IU/L (normal 60–220), thyroid-stimulating hormone (TSH) >100mIU/ml (0.3–4.0) and free thyroxine (T4) <3.0pmol/L (10–20). Urinanalysis showed myoglobin 1.9mg/l (<1) and urine haemoglobin pigments. Serum creatinine was normal, and anti-thyroid peroxidase (TPO) antibodies were negative. He was provisionally diagnosed with hypothyroidism-induced myositis with rhabdomyolysis. He commenced thyroxine replacement therapy, and was treated aggressively with intravenous fluids.
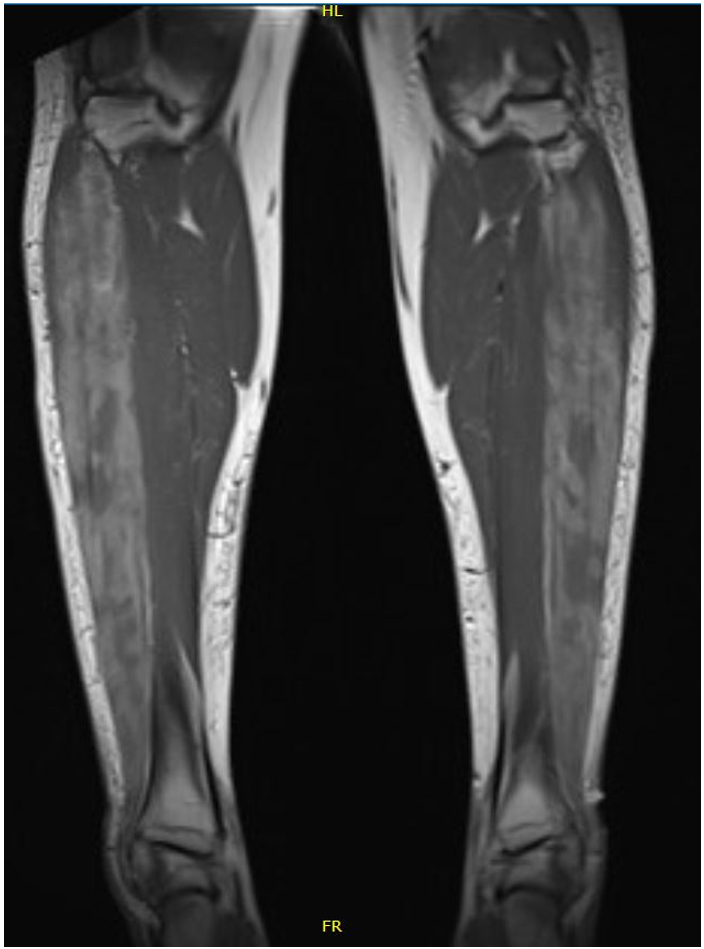
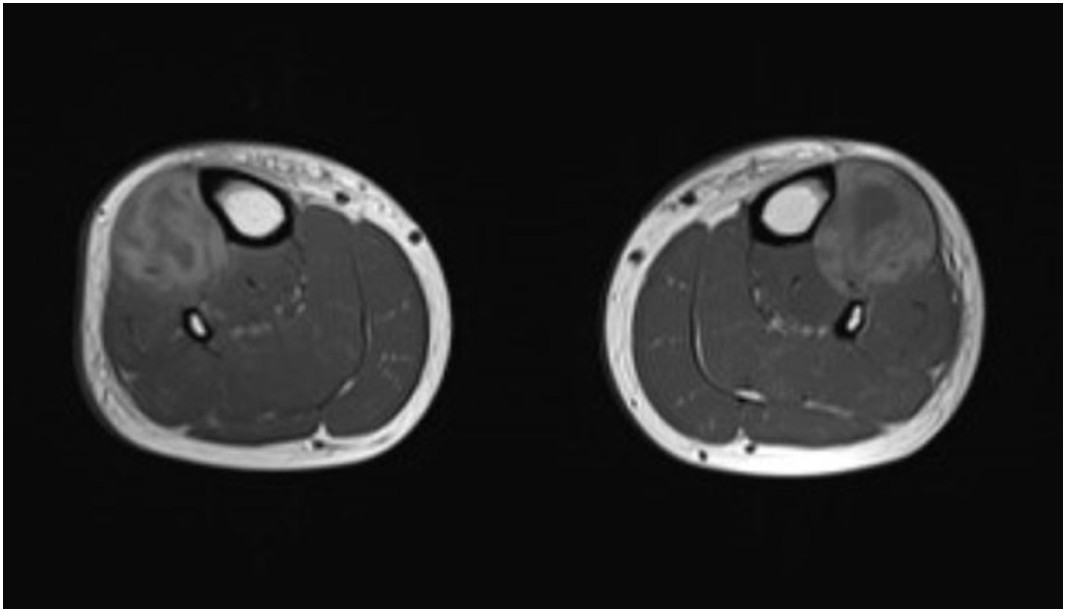
The following day pain worsened with increasing analgesia requirement. Subsequent magnetic resonance imaging (MRI) of the lower limbs confirmed high signal within the muscles of the anterior compartment without any fluid collection, and bulging of the anterior deep fascia (Figure 1). Due to the prolonged duration of symptoms, high likelihood of underlying necrotic tissue with little chance of recovery and risk of post-operative infection, orthopaedic consult advised against performing a fasciotomy. He was discharged for outpatient follow-up with bilateral ankle-foot orthoses and ongoing thyroxine replacement. At six-week follow-up, the anterior compartment discomfort had largely resolved. Thyroid function tests normalised within eight weeks. At six-month follow up, the patient had ongoing bilateral foot drop and is awaiting bilateral tibialis anterior tendon transfers.
Figure 1: T1 sequence magnetic resonance imaging of the lower limbs demonstrating areas of high signal within the muscles in the anterior compartments, consistent with haemorrhage. There is bulging of the anterior deep fascia overlying the anterior compartment and bowing of the interosseous membrane, consistent with increased pressure within the anterior compartment.
Discussion
Although abnormality in thyroid function is a common endocrine disorder, compartment syndrome associated with severe hypothyroidism is rare.1–6 Notably all but one case3 was managed operatively; however, functional outcome was comparable among the other six patients described in the literature. Our case is the youngest adult presentation reported.
The pathophysiology of hypothyroidism-induced myopathy and associated compartment syndrome is incompletely understood. Thyroid hormone is known to exert influence on muscle metabolism, with low levels inducing a mitochondrial driven metabolic myopathy.7 Additional effects include alteration of the actin-myosin unit with changes in regeneration, proliferation and contractility. Further differences in glycosaminoglycan metabolism may lead to abnormal deposition, accumulation and damage. We hypothesise that the combination of abnormal metabolism and function of the muscle cell, coupled with impaired vascularity, lymphatic drainage and oedema due to stimulated fibroblasts predisposed our patient to compartment syndrome, which was precipitated by exercise. Furthermore, increased extracellular fluid accumulation associated with hypothyroidism may be more substantial in the lower limbs due to gravitational effect accounting for presentation in the legs alone.
In contrast to an acute compartment syndrome, our patient had a subacute course over a period greater than 72 hours. Severe pain is often considered a hallmark of compartment syndrome; however, was absent in our patient at the time of presentation.
Additional history obtained from the patient in retrospect did reveal he had suffered from non-specific fatigue for “some years”. It is unclear when he became so grossly hypothyroid, given his normal pubertal development and height. He did not appear to suffer from any additional systemic features of profound hypothyroidism, specifically reduced cardiac function, reduced respiratory or exercise capacity, dermatological or neurological abnormality. The cause for his hypothyroidism is thought most likely to be chronic autoimmune (Hashimoto’s) thyroiditis, despite negative anti-TPO antibodies. He denied any recent flu-like illnesses, fevers or neck discomfort that would suggest acute post viral thyroiditis as the potential aetiology.
This rare case illustrates two points that are generally applicable. Firstly, patients presenting with myopathic symptoms, even in the absence of other typical hypothyroid manifestations should have their thyroid function checked to ensure that occult underlying hypothyroidism is not present. Secondly, early recognition of compartment syndrome that may present in patients without classic risk factors or symptoms is crucial. Symptoms such as an acute foot drop may denote the presence of compartment syndrome and prompt rapid surgical assessment may influence outcomes if recognised early.
Authors
Cameron Schauer, Department of General Medicine, Middlemore Hospital, Counties Manukau District Health Board, Auckland; Young E Koo, Department of General Medicine, Middlemore Hospital, Counties Manukau District Health Board, Auckland; Stephen McBride Department of General Medicine, Middlemore Hospital, Counties Manukau District Health Board, Auckland; Alpesh Patel, Department of Orthopaedic Surgery, Middlemore Hospital, Counties Manukau District Health Board, Auckland.Acknowledgements
We thank Dr Chris Luey from the Department of General Medicine for his insight and contribution into the case, and Dr Mark Rassie from the Department of Radiology, for discussion and review of magnetic resonance images.Correspondence
Dr Cameron Schauer, Department of General Medicine, Middlemore Hospital, Counties Manukau District Health Board, Auckland.Correspondence email
cameron.schauer@gmail.comCompeting interests
Nil.1. Thacker AK, Agrawal D, Sarkari NB. Bilateral anterior tibial compartment syndrome in association with hypothyroidism. Postgrad Med J. 1993; 69:881–3.
2. Hsu SI, Thadhani RI, Daniels GH. Acute compartment syndrome in a hypothyroid patient. Thyroid. 1995; 5:305–8.
3. Muir P, Choe MS, Croxson MS. Rapid development of anterotibial compartment syndrome and rhabdomyolysis in a patient with primary hypothyroidism and adrenal insufficiency. Thyroid. 2012; 22:651–3.
4. Hariri N, Mousa A, Abu-Halimah S, Richmond B. Bilateral lower extremity anterior compartment syndrome in a severely hypothyroid patient. The American surgeon. 2014; 80:E337–8.
5. Musielak MC, Chae JH. Hypothyroid-induced acute compartment syndrome in all extremities. J Surg Case Rep. 2016; 2016.
6. Modi A, Amin H, Salzman M, Morgan F. Acute compartment syndrome caused by uncontrolled hypothyroidism. Am J Emerg Med. 2017; 35:937 e5–e6.
7. Sindoni A, Rodolico C, Pappalardo MA, Portaro S, Benvenga S. Hypothyroid myopathy: A peculiar clinical presentation of thyroid failure. Review of the literature. Rev Endocr Metab Disord. 2016; 17:499–519.
