LETTER
Vol. 133 No. 1511 |
Incidence of Takotsubo syndrome vs acute myocardial infarction in New Zealand (ANZACS-QI 45)
Takotsubo syndrome (TS) (also known as apical ballooning syndrome) is characterised by acute but usually rapidly reversible left ventricular (LV) dysfunction with distinct wall motion abnormalities, predominantly affecting postmenopausal women.
Full article available to subscribers
Takotsubo syndrome (TS) (also known as apical ballooning syndrome) is characterised by acute but usually rapidly reversible left ventricular (LV) dysfunction with distinct wall motion abnormalities, predominantly affecting postmenopausal women.1,2 At presentation TS typically mimics acute myocardial infarction (MI). The reported frequency of TS is 1.0–2.5% in patients presenting with suspected acute MI, and 12% in women presenting with anterior ST-elevation myocardial infarction (STEMI).1 The incidence of TS has been increasing internationally, likely a consequence of an improved awareness of the existence of this syndrome and easier access to early echocardiography and coronary angiography.2–4 Recent international reports suggest that 1–3% of patients (up to 6–9% if only women are considered) with suspected acute coronary syndrome (ACS) have TS.3,5
This study describes the incidence of TS in New Zealand in comparison to MI. Two hundred and fifty-nine TS patients presented to five of the major tertiary hospitals in New Zealand (Middlemore Hospital, Auckland City Hospital, North Shore Hospital, Christchurch Hospital and Dunedin Hospital) between January 2015 and June 2018 were included. Only patients who underwent angiography (either cardiac CT angiography [n=27] or invasive coronary angiography [n=232]) were included. TS was defined using the International Takotsubo Diagnostic Criteria (InterTAK Diagnostic Criteria).6 TS cases were subdivided according to the presentation ECG—ST-elevation TS (STE-TS) or non-ST-elevation TS (NSTE-TS).7
The MI cohort comprised of all patients who presented to the participating hospitals with acute MI between over the same time period. A total of 11,900 of patients (8,405 men and 3,495 women) with STEMI and non-ST-myocardial infarction (NSTEMI) were identified. The data was extracted from the All New Zealand Acute Coronary Syndrome Quality Improvement (ANZACS-QI) registry.8 This registry captured almost all New Zealand public hospital coronary angiography procedures, including those associated with an acute coronary syndrome (ACS) diagnosis.9 Only patients who had coronary angiography were included to ensure comparability with the TS cohort.
The demographic characteristics of the TS and MI populations are summarised in Table 1; 96.1% (n=249) of the TS patients were women (n=249, 96.1%) with median age of 66 years (IQR 57–73 years). They were slightly younger than MI females. Majority of both cohorts were European. Two-thirds of female TS cohort presented without ST-segment elevation and they had less conventional cardiovascular risk factors compared to the female MI cohort. A stressful trigger (defined as an unusual emotional or physical stress occurring before symptom onset) was identified in 190 patients (73.4%); 117 had an emotional stressor and 73 reported a physical stressor (defined as medical conditions that trigger TS).
Table 1: Clinical characteristics of patients with Takotsubo syndrome versus patients with myocardial infarction.
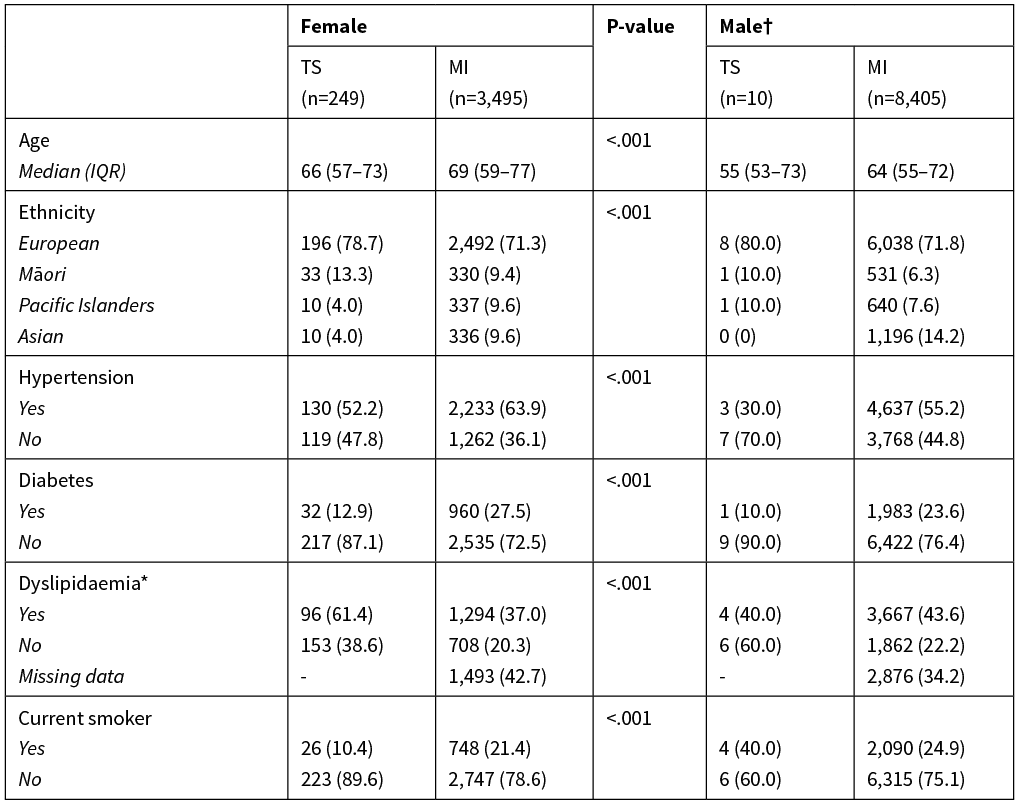

*The missing data has been excluded in the comparison.†P values for comparison between men with TS and men with MI are not given due to the small number of men with TS.ACS, acute coronary syndrome; TS Takotsubo syndrome; CVD, cardiovascular disease; STEMI, ST elevation myocardial infarction; NSTEMI, non-ST elevation myocardial infarction; STE-TS, ST elevation Takotsubo syndrome; NSTE-TS, Non ST elevation Takotsubo syndrome; 3VD; 3 vessels disease; LMS, left main stem disease, LVEF, left ventricular ejection fraction.
A reduced left ventricular ejection fraction (LVEF), defined as LVEF<50% was noted in 84.3% of TS women on admission but in only 28.5% of women with MI. More than half of women with TS had LVEF<40% on admission. Thirty-one female TS patients had coronary artery disease documented on either invasive coronary angiography (n=6) or CT coronary angiography (n=25). Of note, 19.9% of women with a diagnosis of MI had no obstructive coronary artery disease (defined as <50% epicardial coronary stenosis in all major epicardial coronary arteries).
The numbers of women with TS and MI in five of the major tertiary hospitals in New Zealand are presented in Table 2. Between 1 January 2015 and 30 June 2018, 259 patients (249 females and 10 men) had TS. Over this period, 3,495 women and 8,405 men presented with MI. The proportions with TS, of those with MI or TS, were therefore 6.6% for women and 0.1% for men. Two-thirds of the female TS patients (n=167) presented without ST-segment elevation. The proportion of TS in women with NSTEMI/NSTEACS was 6.3%, and in women with STEMI/STE-TS was 7.5%. Overall, 2.2% of the MI/TS cohort had TS. The InterTAK investigators reported an overall prevalence of 4.1% in an ACS registry in Zurich hospitals10 and the incidence of TS in women with suspected MI has been found to be 5.9–7.5%.11 Even in this contemporary New Zealand MI cohort, women were three times more likely than men to have non-obstructive coronary artery disease. At least some of those patients may have been misdiagnosed as ACS, particularly if echocardiography was delayed. TS diagnosis requires identification of typical LV wall motion abnormalities, which are relatively transient. If imaging is delayed and they have resolved, the default diagnosis is likely to be MI. If a third of these 696 women were reclassified as TS it would nearly double our estimated number with TS.
Table 2: Numbers of MI and TS cases and the proportion with TS—female sub-cohort and overall cohort (female and male).
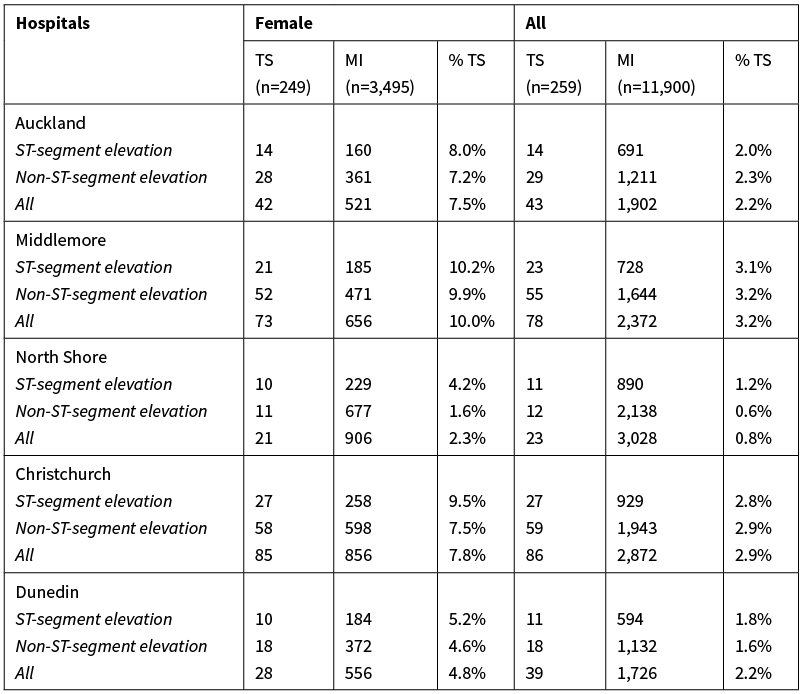
TS, Takotsubo syndrome; MI, myocardial infarction.
The proportion with TS varies among the five hospitals, ranging between 2.3–10.0%. The proportion of women with STEMI/STE-TS who had TS was 4.2–10.2%, and of those with NSTEMI/NSTE-ACS it was 1.6–9.9%. Of note, the proportion of women at Middlemore Hospital with TS was 10.0%. This seems high compared to the other four hospitals. Because Middlemore Hospital has had an active interest in TS for many years and maintains a prospective registry, it is likely that very few TS diagnoses are missed, which may in part account for the higher proportions. The proportion of TS/MI patients with TS in Christchurch hospital was 7.8%. Following the major Christchurch and Kaikoura earthquakes, Christchurch Hospital has seen unprecedented case clusters of TS, which accounts for the higher level observed.12
Two extensive overviews of American TS cohorts found that anxiety and chronic stress were both associated with significantly higher odds of developing TS.13,14 Depression has also been reported to be associated with higher odds of developing TS. The increased prevalence of premorbid psychiatric diagnoses, particularly anxiety disorders and depression in TS patients suggests a potential link between neuropsychiatric disorders and TS. In particular, the Canterbury earthquakes had significant adverse impact on mental health, which could account for the high incidence observed.
It is difficult to estimate the frequency of TS in the general population. Indeed, the true incidence of TS may still be underestimated because TS may be misdiagnosed as ACS. It is still unclear if the extent to which the growing numbers increase in incidence compared with prior reports reflects an increasing awareness of this syndrome by clinicians or if it is in fact a true rise in its incidence. Nevertheless, it is worth remembering that TS is not rare and heightened awareness of this condition will likely lead to a higher reported incidence.
Authors
Jen-Li Looi, Department of Cardiology, Middlemore Hospital, Otahuhu, Auckland; Toby Verryt, Department of Cardiology, Christchurch Hospital, Christchurch; Peter McLeod, Department of Cardiology, Dunedin Hospital, Dunedin; Christina Chan, Department of Cardiology, Dunedin Hospital, Dunedin; James Pemberton, Department of Cardiology, Dunedin Hospital, Dunedin; Mark Webster, Green Lane Cardiovascular Service, Auckland City Hospital, Auckland; Andrew To, Cardiovascular Division, North Shore Hospital, Takapuna, Auckland; Mildred Lee, Department of Cardiology, Middlemore Hospital, Otahuhu, Auckland; Andrew J Kerr, Department of Cardiology, Middlemore Hospital, Otahuhu, Auckland.Correspondence
Jen-Li Looi, Department of Cardiology, Middlemore Hospital, Private Bag 93311, Otahuhu, Auckland.Correspondence email
jenli.looi@middlemore.co.nzCompeting interests
Nil.1. Parodi G, Del Pace S, Carrabba N, Salvadori C, Memisha G, Simonetti I, et al. Incidence, clinical findings, and outcome of women with left ventricular apical ballooning syndrome. Am J Cardiol. 2007; 99(2):182–5.
2. Templin C, Ghadri JR, Diekmann J, Napp LC, Bataiosu DR, Jaguszewski M, et al. Clinical Features and Outcomes of Takotsubo (Stress) Cardiomyopathy. N Engl J Med. 2015; 373(10):929–38.
3. Lyon AR, Bossone E, Schneider B, Sechtem U, Citro R, Underwood SR, et al. Current state of knowledge on Takotsubo syndrome: a Position Statement from the Taskforce on Takotsubo Syndrome of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2016; 18(1):8–27.
4. Minhas AS, Hughey AB, Kolias TJ. Nationwide Trends in Reported Incidence of Takotsubo Cardiomyopathy from 2006 to 2012. Am J Cardiol. 2015; 116(7):1128–31.
5. Parodi G, Bellandi B, Del Pace S, Barchielli A, Zampini L, Velluzzi S, et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011; 139(4):887–92.
6. Ghadri JR, Wittstein IS, Prasad A, Sharkey S, Dote K, Akashi YJ, et al. International Expert Consensus Document on Takotsubo Syndrome (Part I): Clinical Characteristics, Diagnostic Criteria, and Pathophysiology. Eur Heart J. 2018; 39(22):2032–46.
7. Looi JL, Wong CW, Lee M, Khan A, Webster M, Kerr AJ. Usefulness of ECG to differentiate Takotsubo cardiomyopathy from acute coronary syndrome. Int J Cardiol. 2015; 199:132–40.
8. Kerr A, Williams MJ, White H, Doughty R, Nunn C, Devlin G, et al. The All New Zealand Acute Coronary Syndrome Quality Improvement Programme: Implementation, Methodology and Cohorts (ANZACS-QI 9). N Z Med J. 2016; 129(1439):23–36.
9. Kerr AJ, Lee M, Jiang Y, Grey C, Wells S, Williams M, et al. High level of capture of coronary intervention and associated acute coronary syndromes in the all New Zealand acute coronary syndrome quality improvement cardiac registry and excellent agreement with national administrative datasets (ANZACS-QI 25). N Z Med J. 2019; 132(1492):19–29.
10. Ghadri JR, Cammann VL, Jurisic S, Seifert B, Napp LC, Diekmann J, et al. A novel clinical score (InterTAK Diagnostic Score) to differentiate takotsubo syndrome from acute coronary syndrome: results from the International Takotsubo Registry. Eur J Heart Fail. 2017; 19(8):1036–42.
11. Sy F, Basraon J, Zheng H, Singh M, Richina J, Ambrose JA. Frequency of Takotsubo cardiomyopathy in postmenopausal women presenting with an acute coronary syndrome. Am J Cardiol. 2013; 112(4):479–82.
12. Chan C, Troughton R, Elliott J, Zarifeh J, Bridgman P. One-year follow-up of the 2011 Christchurch Earthquake stress cardiomyopathy cases. N Z Med J. 2014; 127(1396):15–22.
13. Summers MR, Lennon RJ, Prasad A. Pre-morbid psychiatric and cardiovascular diseases in apical ballooning syndrome (tako-tsubo/stress-induced cardiomyopathy): potential pre-disposing factors? J Am Coll Cardiol. 2010; 55(7):700–1.
14. Mudd JO, Kapur NK, Champion HC, Schulman SP, Wittstein IS. Patients with Stress-Induced (Takotsubo) Cardiomyopathy Have an Increased Prevalence of Mood Disorders and Antidepressant Use Compared to Patients with Acute Myocardial Infarction. Journal of Cardiac Failure. 2007; 13(6):S176.
